Air Embolism
Vascular air embolism is the entrainment of air (or exogenously delivered gas) from the operative field or other communications with the environment into the venous or arterial vasculature, producing systemic effects.1
Did you Know?

(1) Ho, Anthony M.-H. Is Emergency Thoracotomy Always the Most Appropriate Immediate Intervention for Systemic Air Embolism After Lung Trauma? CHEST (1999), Volume 116 , Issue 1 , 234 - 237
Causes
There are common causes of air embolism in different clinical processes and most of them are of iatrogenic nature.1,2
- Entering of air through open IV access and infusion systems (e.g. open stop cock, disconnection, leakage due to product failure). The amount of air entry is influenced by the position of the patient and height of the vein with respect to the right side of the heart.1,2,3
- Not properly filled and completely vented infusion line.3
- Parallel infusions, where gravity infusions and infusion pumps are connected together and interact through the infusion lines. Such systems can develop a beading (fluid-air-fluid etc.), when the gravity infusion runs dry (Fig. 1).4
- During various surgical interventions, especially neurosurgical, vascular, obstetric, gynecological, or orthopedic procedures by the opened vascular system.5,6
- Incorrect execution of procedures for pressure infusion.7,8
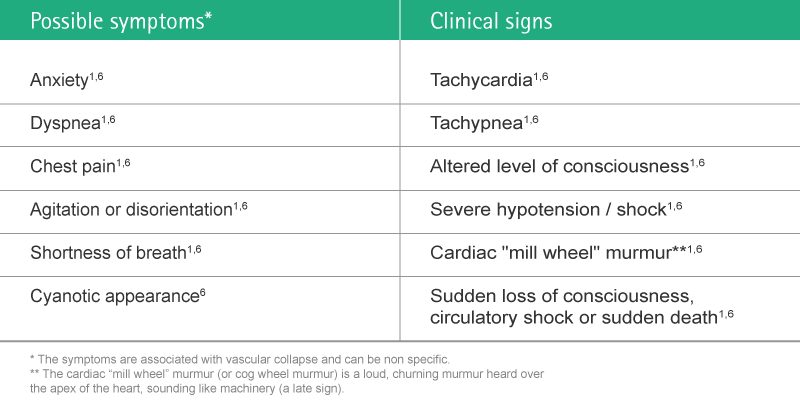
Health Consequences
The symptoms and clinical signs of air embolism are related to the degree of air entry into the circulation system. They usually develop immediately after embolization.1
Complications
It is generally accepted that any amount of air that might enter the patient must be considered critical. The impact is directly correlated with the patient’s condition, the volume of air and the rate of accumulation.1
Clinical complications are diminished cardiac output, shock and death.1,6
Financial Consequences
Preventing the entrance of air into the patient’s circulatory system can result in tangible budget savings for the healthcare provider.
A cost evaluation of the risk can be done by assigning costs to their related clinical treatment and resulting extended length of stay. The cost can be calculated using the average daily cost of the expected clinical treatment.
Potential Risk Associated Cost
The Fig. 3 below shows an estimation of possible additional costs as a consequence of complications caused by air embolism. In order to facilitate the attribution of each complication to the cost calculation, severity levels were introduced.
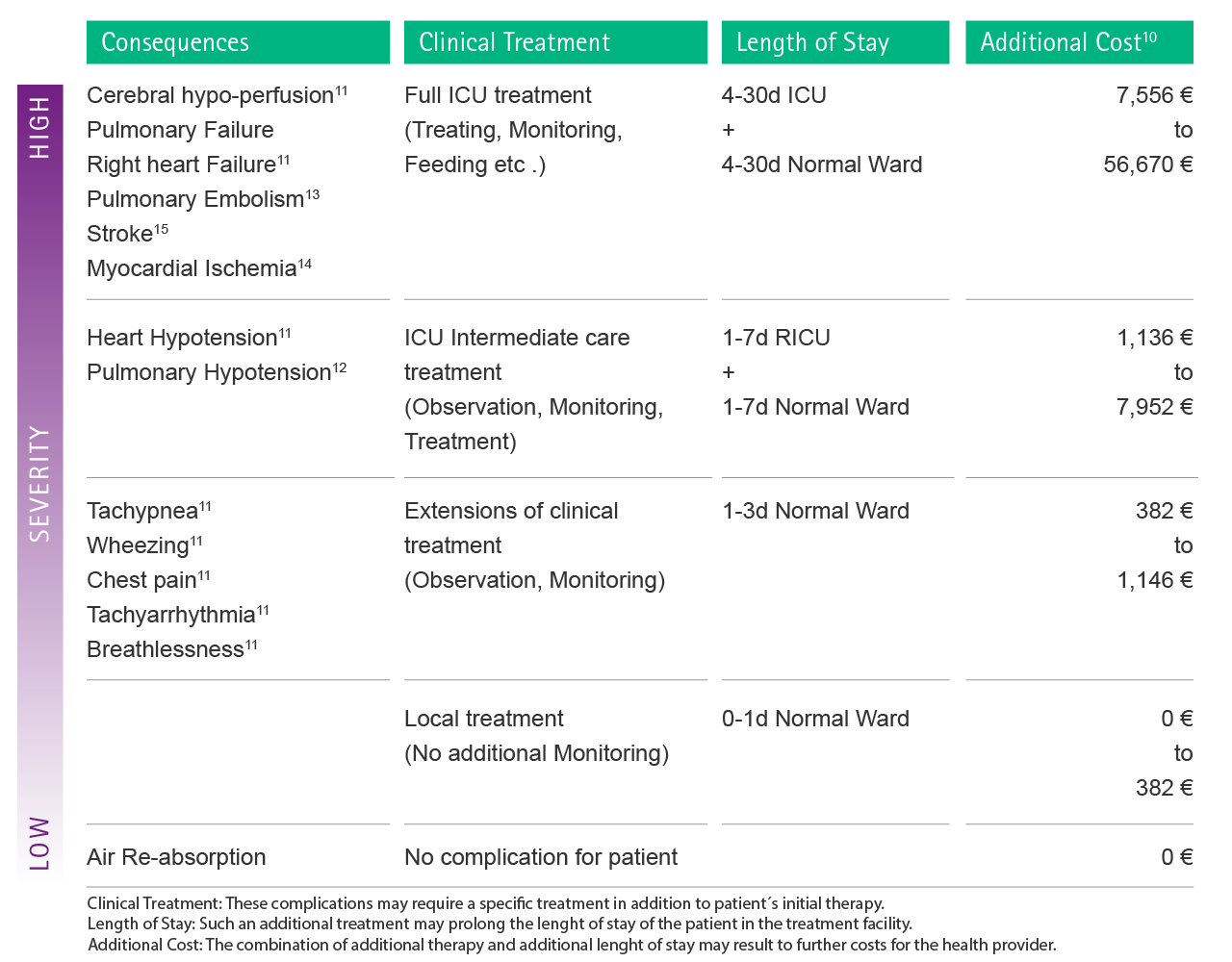
In the case of severe multiple complications which require full ICU treatment, a hospital may save up to 56,670 € per single case.11-15
Even non-fatal episodes of venous air embolism lead to extensive involvement for diagnostic (e.g. blood gas analysis, echocardiography, ultrasonography) and therapeutic interventions (e.g. oxygen, intravascular volume expansion, catecholamines).11
Preventive Strategies
To prevent air embolism and ensure safe patient treatment it is important to combine various strategies and actions in different processes.
- For the placement of a peripheral cannula, the risk of air embolism can be reduced by ensuring that the selected arm of the patient is kept below the level of the heart during the insertion or removal procedure.1,2
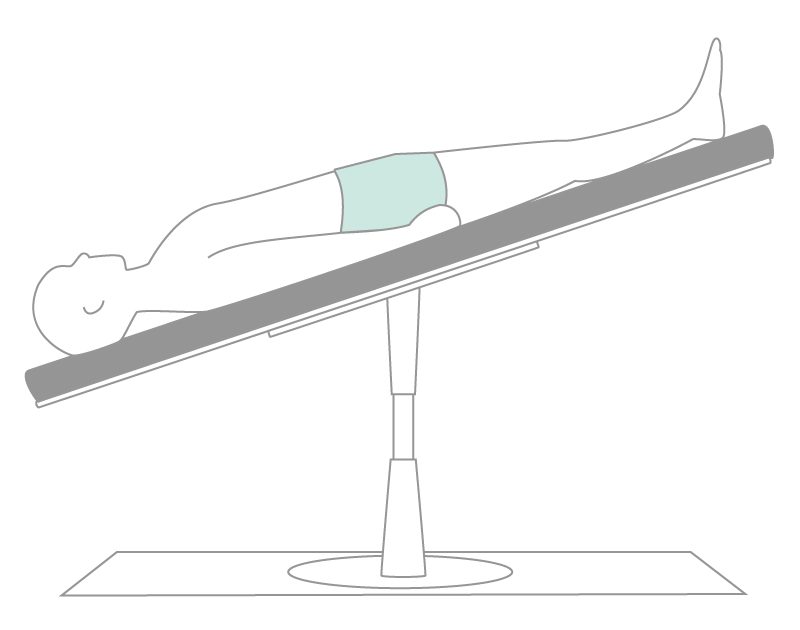
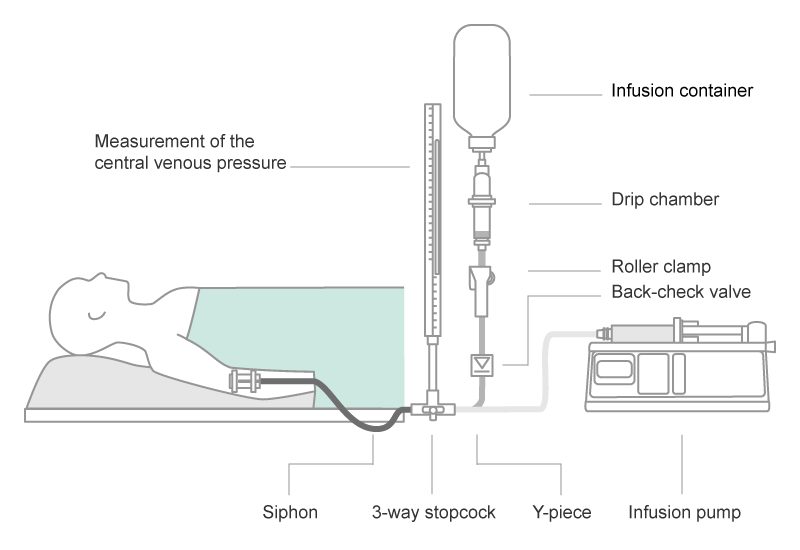
- For the central venous catheter, the best position for its insertion or removal is in the supine or Trendelenburg position. This minimizes the risk of air embolism (Fig. 4).1,2
- Usage of Luer-Lock connections minimizes the potential for the accidental disconnection of administration sets and syringes from intravenous catheters.1,2
- Leaking infusion tubes should be changed immediately to eliminate the risk of air being drawn into the vascular system.1
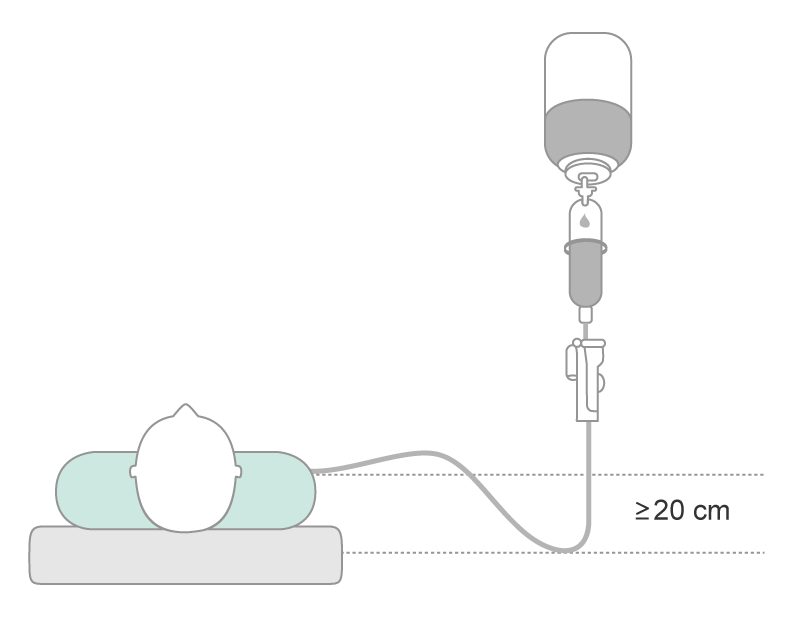
- Infusion regimens should always be set up to create a siphon ( ≥ 20 cm) in the infusion system, which protects against the ingress of air (Fig. 5).9
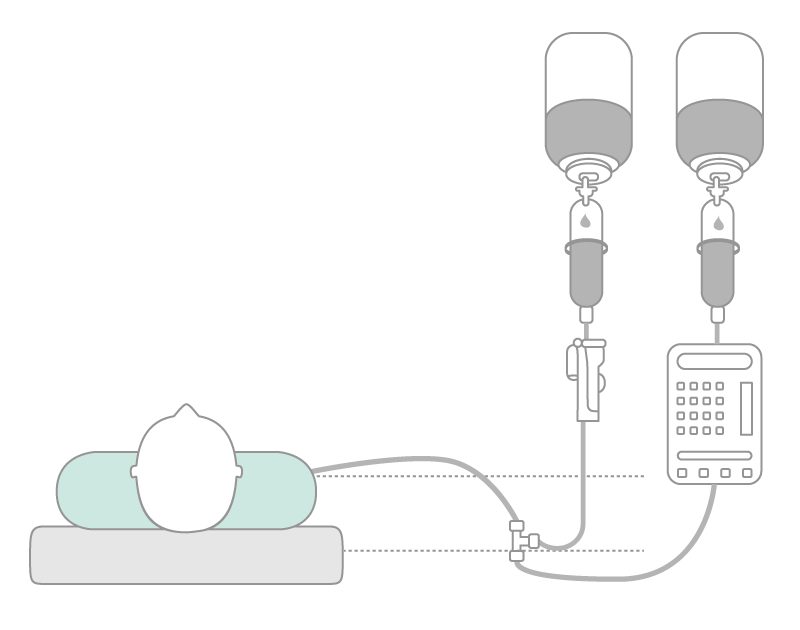
- In parallel infusions, the three-way stopcock of the bypass should be placed in the ascending siphon tube. Use a back check valve for gravity infusions (Fig. 6).
- Modern infusion filters are able to separate 100% of air from infusion lines in addition to the removal of particles and bacteria.9,10
- Usage of modern infusion sets featuring an air stop mechanism.9
Highlight Safety Products
Scientific Evidence
1 Cook LS. (2013) Infusion-related air embolism. J Infus Nurs; 36(1): 26-36
2 Gabriel J. (2008) Infusion therapy. Part two: Prevention and management of complications. Nurs Stand; 22(32): 41-8
http://www.ncbi.nlm.nih.gov/pubmed/18481602%20
3 Lee PT, Thompson F, Thimbleby H. (2012) Analysis of infusion pump error logs and their significance for health care. Br J Nurs; 21(8): S12, S14, S16-20
4 Obermayer A. (1994) Physikalisch-technische Grundlagen der Infusionstechnik – Teil 2. Medizintechnik; 114(5): 185-190
5 Agarwal SS, Kumar L, Chavali KH, Mestri SC. (2009) Fatal venous air embolism following intravenous infusion. J Forensic Sci; 54(3): 682-4
6 Wittenberg AG. (2006) Venous Air Embolism. Emedicine 2006
7 Zoremba N, Gruenewald C, Zoremba M, Rossaint R, Schaelte G. Air elimination capability in rapid infusion systems. Anaesthesia; 66(11): 1031-4
8 Suwanpratheep A, Siriussawakul A. (2011) Inadvertent venous air embolism from pressure infuser bag confirmed by transesophangeal echocardiography. J Anesthe Clinic; 2:2-10
9 Riemann T. (2004) How many “milliliters” of air will leas to an air-embolism? Die Schwester Der Pfleger; 8: 594-595
10 Jack T, Boehne M, brent BE, hoy L, Köoditz H, wessel A, Sasse M. (2012) In-line filtration reduces severe complications and length of stay in pediatric intensive care unit: a prospective, randomiyed controlled trial. Intensive Care Med: 38(6): 1008-16
11 Mirski et al.2007, Perdue 2001, Wittenberg 2006 Diagnosis and treatment of vascular air embolism. Anesthesiology 2007; 106(1): 164-77
http://www.ncbi.nlm.nih.gov/pubmed/17197859
12 Josephson DL. Risks, complications, and adverse reactions associated with intravenous infusion therapy. In: Josephson DL. Intravenous infusion therapy for medical assistants.
The American association of Medical Assistants. Clifton Park: Thomson Delmar Learning 2006; 56-82
http://www.chegg.com/textbooks/intravenous-infusion-therapy-for-medical-assistants-1st-edition-9781418033118-1418033111
13 Souders JE. Pulmonary air embolism. J Clin Monit Comput 2000; 16(5-6): 375-83
http://www.ncbi.nlm.nih.gov/pubmed/12580220
14 Lamm G, Auer J, Punzengruber C, Ng CK and Eber B. Intracoronary air embolism in open heart surgery – an uncommon source of myocardial ischaemia. Int J Cardiol 2006; 112(3): 85-6
http://www.ncbi.nlm.nih.gov/pubmed/16887218
15 Demaerel P, Gevers AM, De Bruecker Y, Sunaert S and Wilms G.
Gastrointest Endosc. Stroke caused by cerebral air embolism during endoscopy 2003; 57(1): 134-5
http://www.ncbi.nlm.nih.gov/pubmed/12518155
16 Ho, Anthony M.-H. Is Emergency Thoracotomy Always the Most Appropriate Immediate Intervention for Systemic Air Embolism After Lung Trauma? CHEST (1999), Volume 116 , Issue 1 , 234 - 237