Misplacement and Malposition of Central Venous Access Devices
Definitions:
CVAD
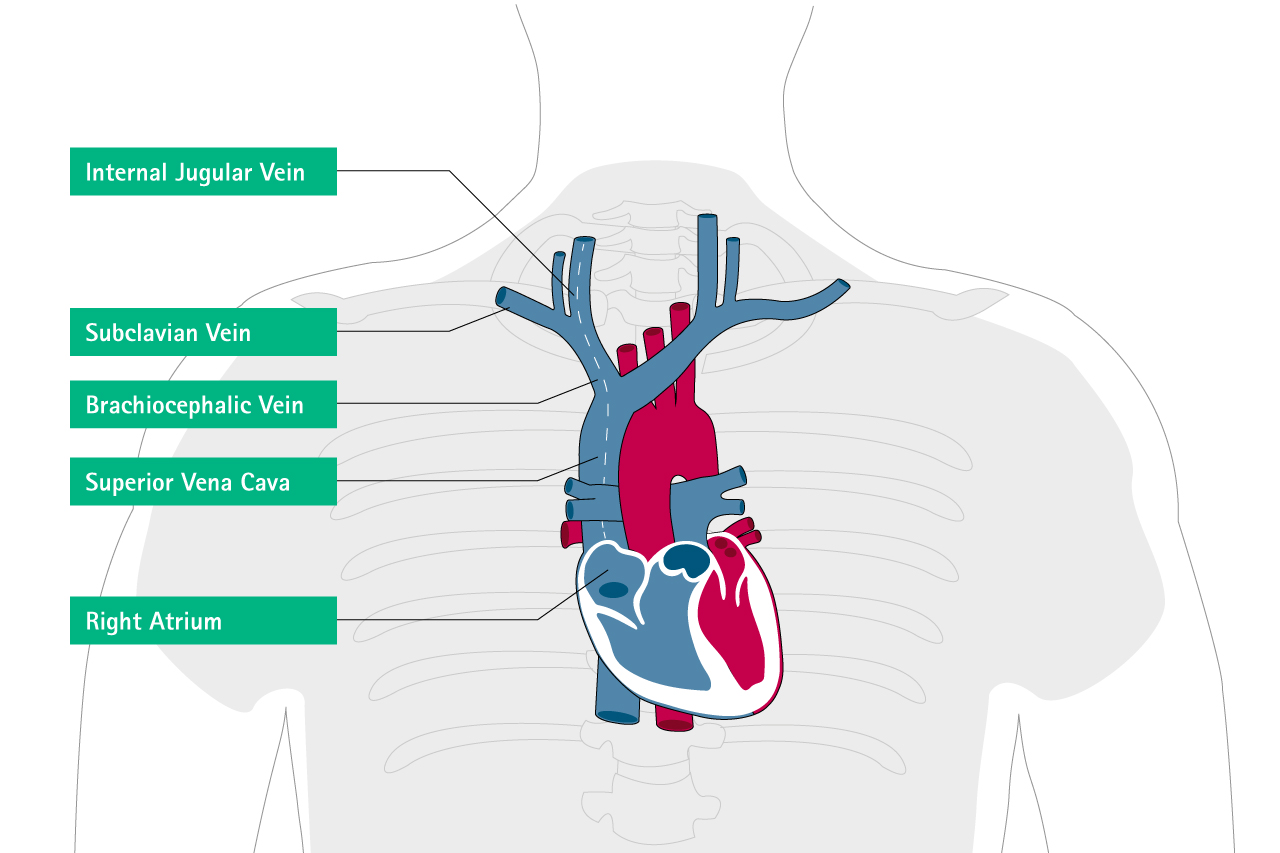
Central venous access devices (CVADs) are used for short or long-term infusion of fluids, medications and monitoring, or when establishing a peripheral venous access is not possible or difficult.CVADs can be inserted into the subclavian or jugular vein as centrally inserted central venous catheters (CICCs or conventionally called CVCs), totally implanted venous access devices (TIVAD conventionally called access ports AP), or can be inserted into one of the peripheral veins of the upper extremities, called peripherally inserted central catheters (PICCs).1
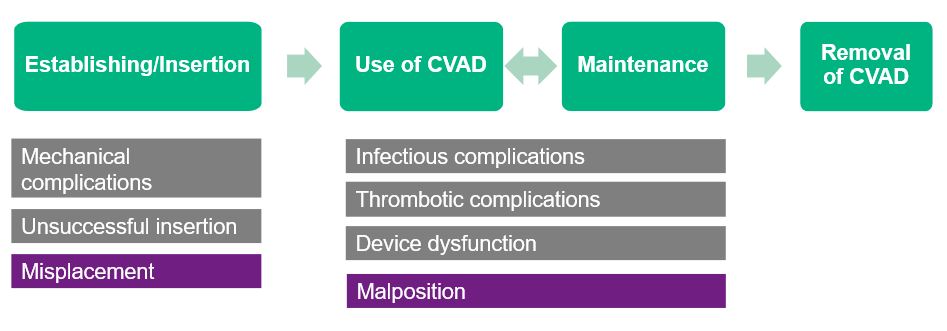
Misplacement and Malposition of CVAD
The misplacement or malposition of centrally and peripherally inserted central venous catheters describes the improper location of the catheter tip.2,3
Did you Know?
Where is the “ideal” catheter tip location and how do you place the catheter tip correctly?
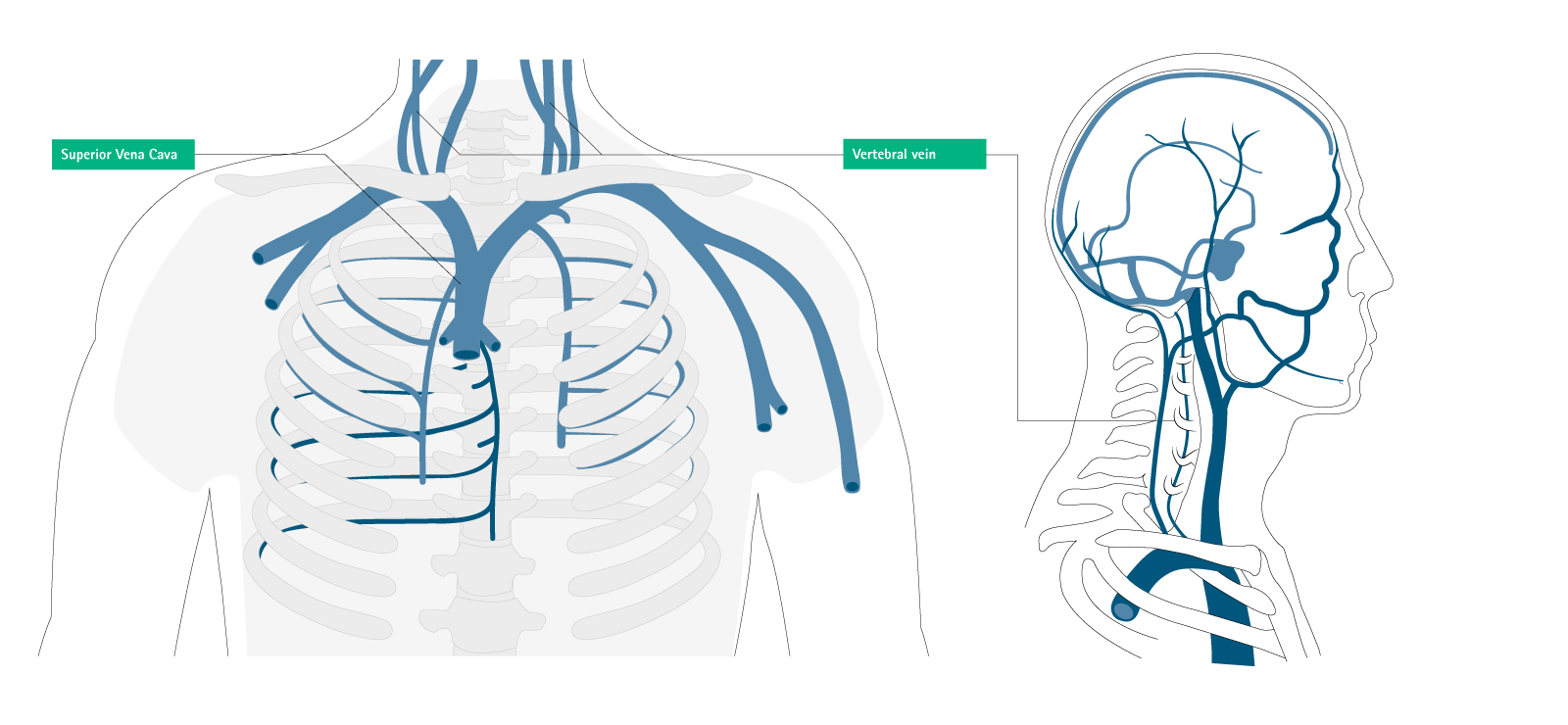
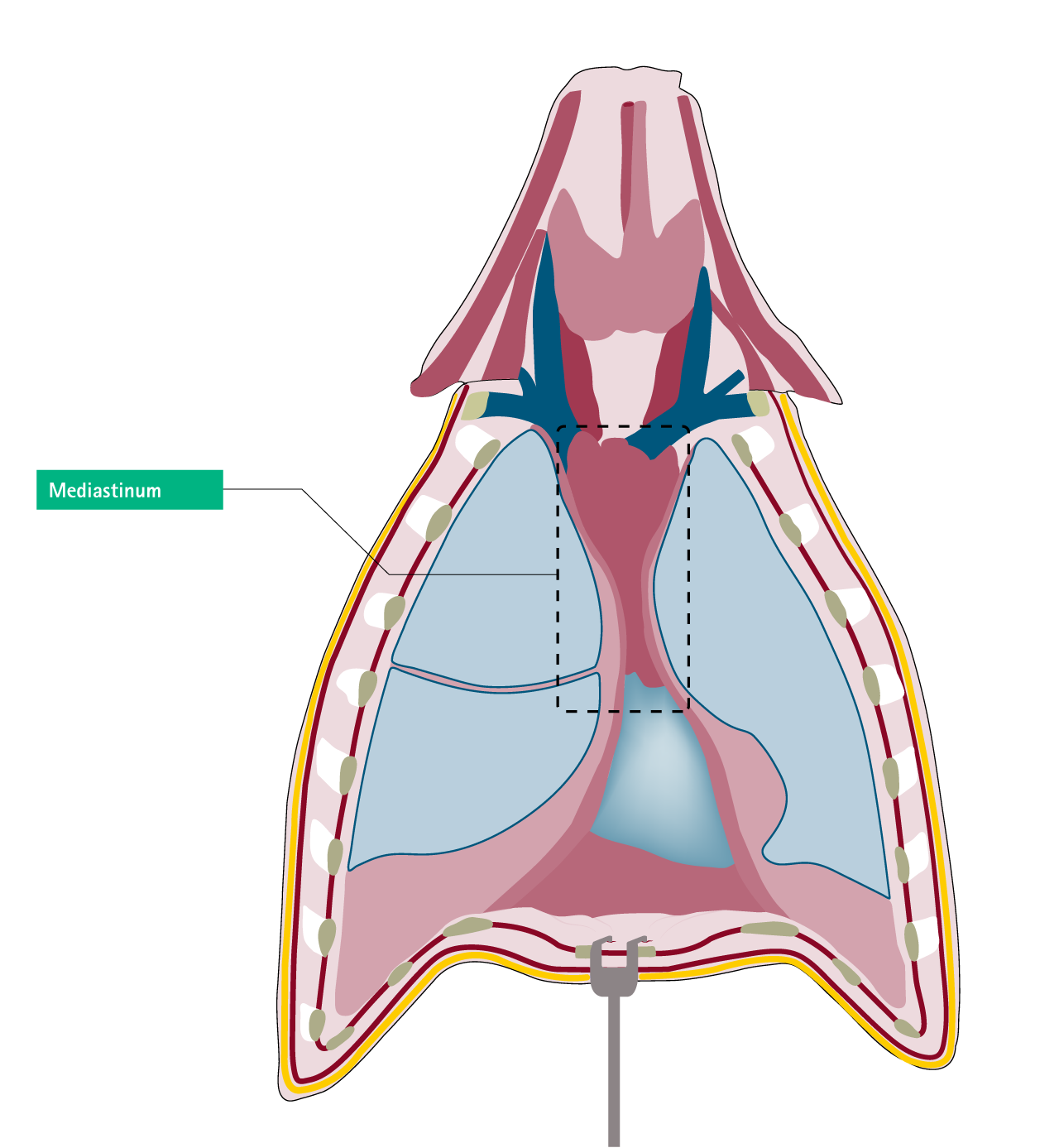
“The tip of the catheter should be in a central vein (Superior Vena Cava, SVC, or Inferior Vena Cava, IVC), close to the cavoatrial junction.”1
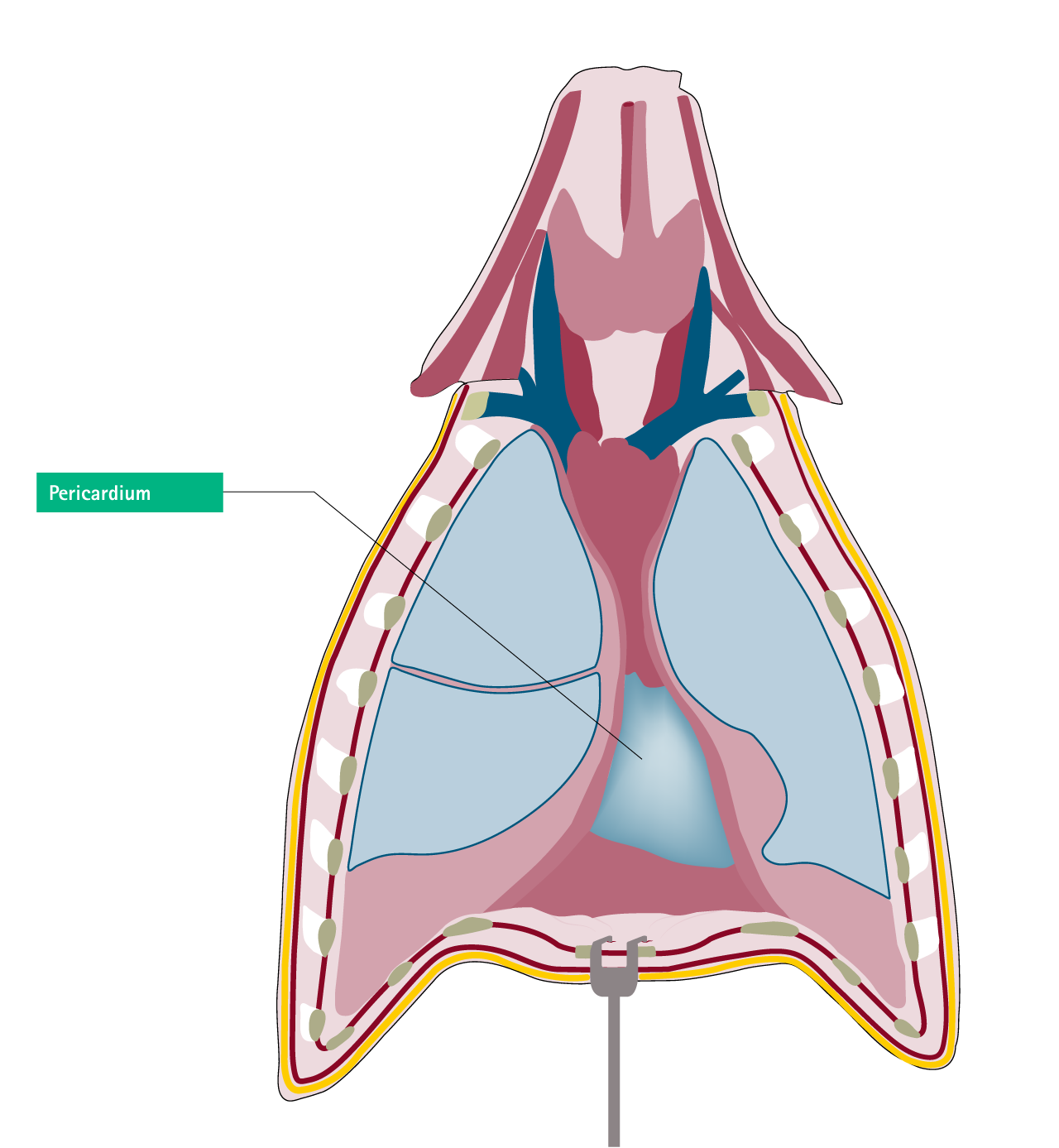
- Ideally outside of the pericardial sac
- Parallel with the long axis of the vein
- The tip does not abut the vein or heart wall at an acute angle or end on3,4
- The ideal catheter position is the area between the lower third of vena cava superior and upper the third of right atrium5
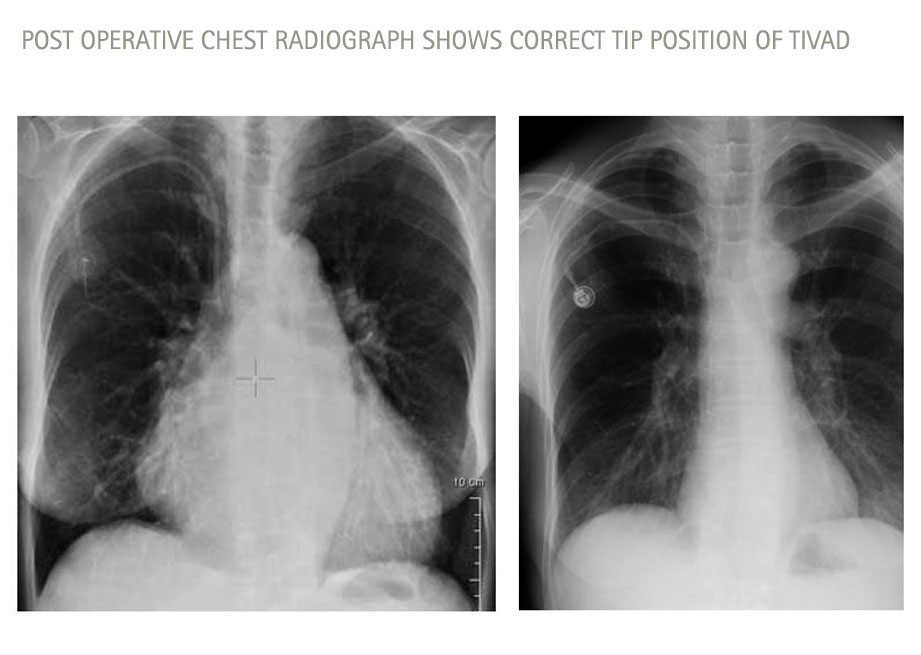
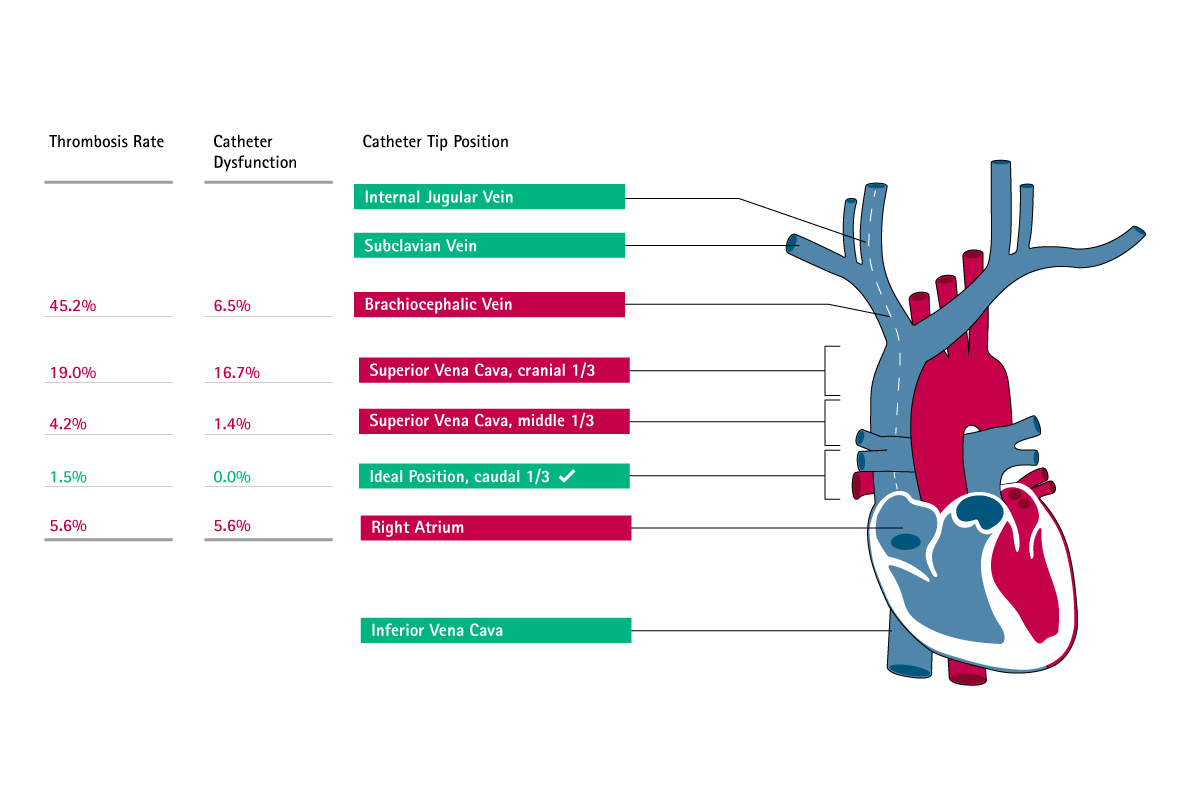
Correct catheter tip positioning6
Conclusion:
„…correct position of the catheter has to be ensured during placement
Caers J, Fontaine C,Vinh-Hung V et al (2005) Catheter tip position as a risk factor for thrombosis associated with the use of subcutaneous infusion ports. Support Care Cancer 13:325-331
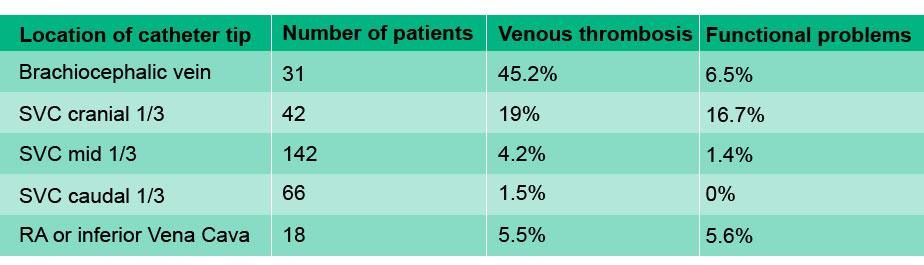
Relation between catheter tip position an complication rate
| Location of catheter tip position | Number of patients | Venous thrombosis | Functional problems |
| Brachiocephalic vein | 31 | 45.2% | 6.5% |
| SVC cranial 1/3 | 42 | 19% | 16.7% |
| SVC mid 1/3 | 142 | 4.2% | 1.4% |
| SVC caudal 1/3 | 66 | 1.5% | 0% |
| RA or inferior Vena Cava | 18 | 5.5% | 5.6% |
Why is it important to achieve an "ideal" catheter tip location for CVC, TIVAD and PICC?
- Infusion of vasopressors, irritant drugs, or parenteral nutrition requires maximal dilution, avoiding mixing of multiple drugs such as chemo- and antibiotic therapy and blood sampling
- Extracorporeal circuits, e.g. dialysis requires a very high blood flow rate passing by the catheters, and separation of inflow and outflow of catheters to avoid blood recirculation
- Measurement of ScvO2 requires catheter tip lies in or as close to the right atrium as possible
Misplacement/Malposition is one of the most common complications related to CVADs7-10
Misplacement/Malposition could occur in different CVAD application
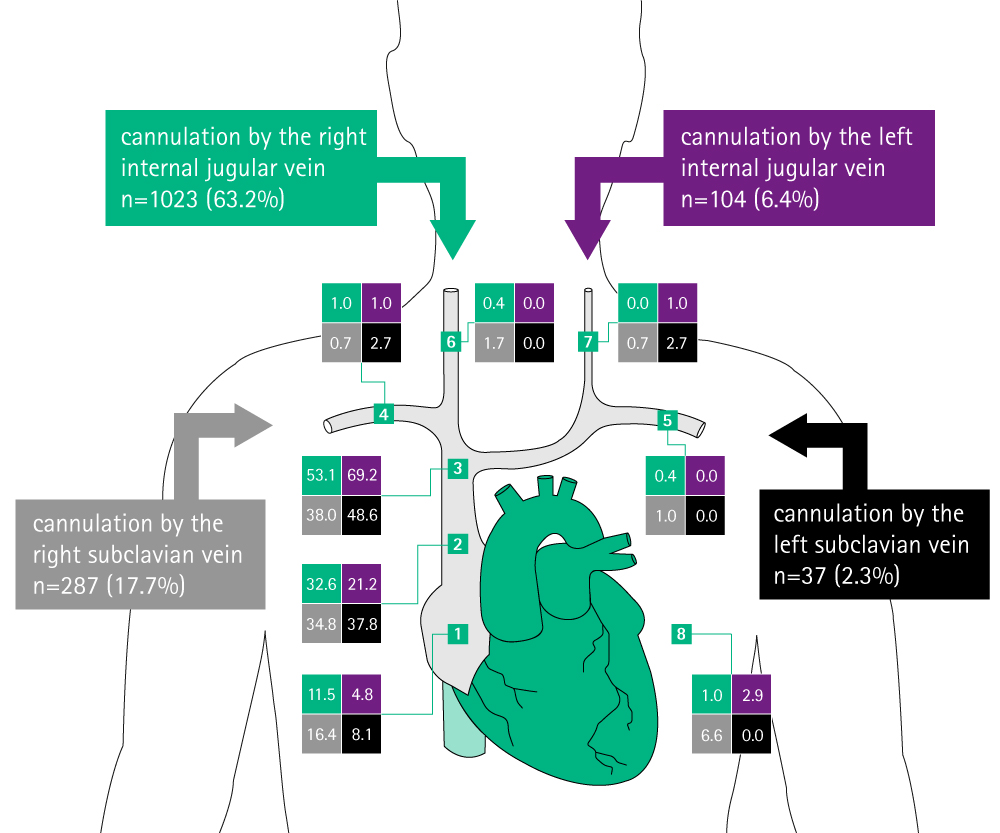
Catheter tip positions in the real practice
Catheter tip positions are shown in percent of the total number of cannulations at each puncture site.
- 1. Right atrium.
- 2. Caudal third of superior vena cava (SVC).
- 3. Cranial two-thirds of SVC or brachiocephalic veins.
- 4. Intrathoracic part of the right subclavian vein.
- 5. Intrathoracic part of the left subclavian vein.
- 6. Right internal jugular vein.
- 7. Left internal jugular vein.
- 8. Other Graphic adapted from Pikwer A, et al. Anaesth Intensive Care. 2008; 36:30–712
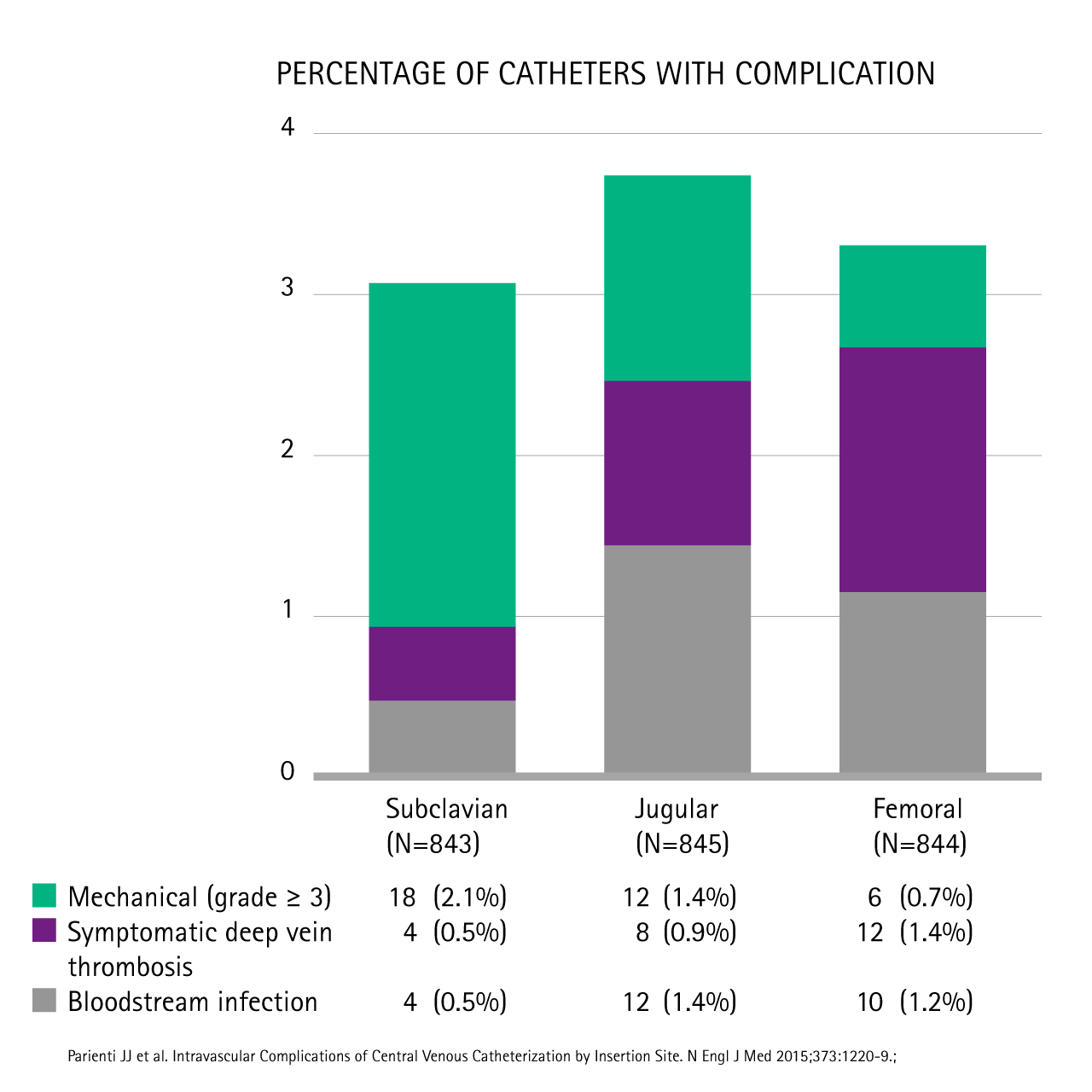
Incidence of CVC complication (%) vs. puncture site
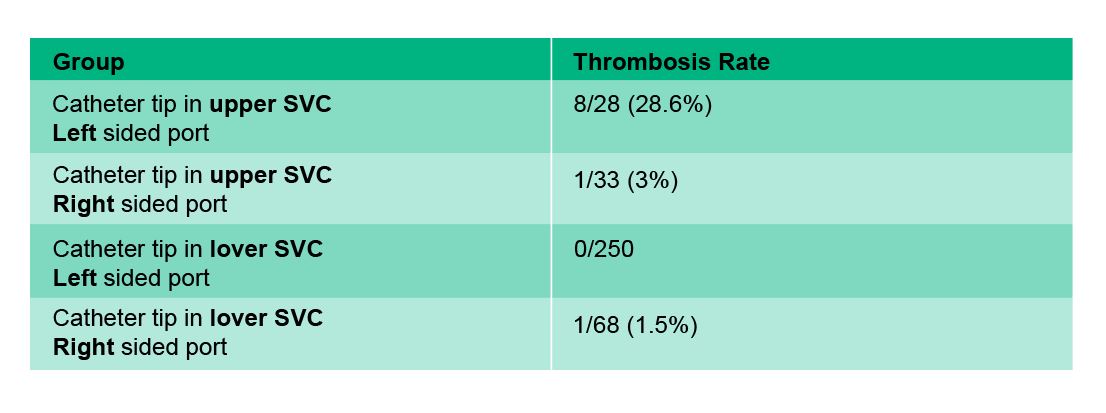
Importance of correct catheter tip positioning for TIVADs & PICCs
Clinical needs:
- Access Port catheters might remain in situ for several years!
- Therefore, correct and accurate positioning of the catheter is important
- Incorrect positioning can lead to a higher rate of long term complications (e.g. thrombosis)*
*Superior vena cava thrombosis related to catheter malposition in cancer chemotherapy given through implanted ports.
.Puel V, Caudry M, Le Métayer P, Baste JC, Midy D, Marsault C, Demeaux H, Maire JP.Cancer. 1993 Oct 1;72(7):2248-52.
Conclusion:
„…patients with left-sided port and catheter tips lying in the upper part of the vena cava are at high risks for severe thrombotic complications.“
Relation between catheter tip position and complication rate
Support Care Cancer, 2005 May; 13(5):325-31, Epub 2004 Nov 5.
Catheter tip position as a risk factor for thrombosis associated with the use of subcutaneous infusion ports.
Caers J1, Fontaine C, Vinh-Hung V, De Mey J, Ponnet G, Oost C, Lamote J, De Greve J, Van Camp B, Lacor P
Causes
Potential Causes of Catheter Misplacement
Patient factors
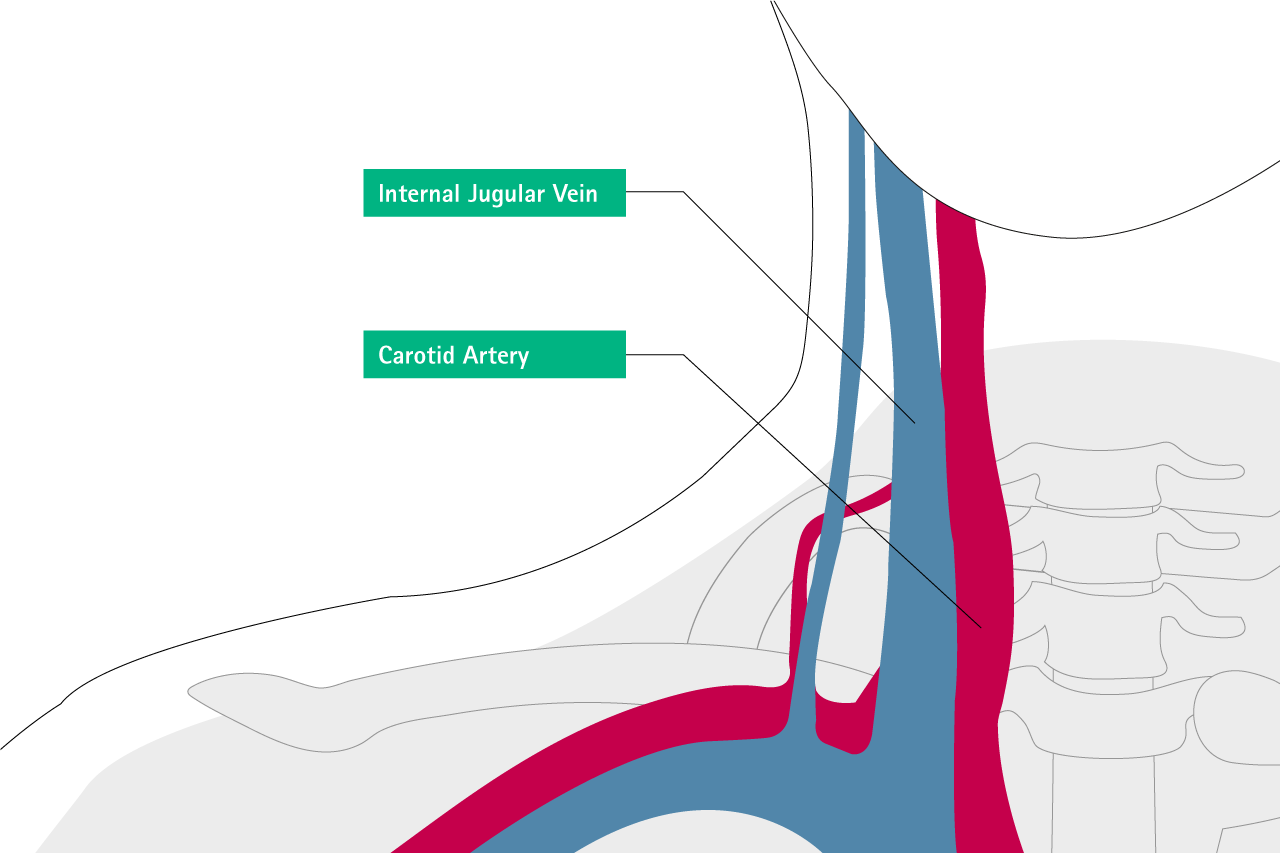
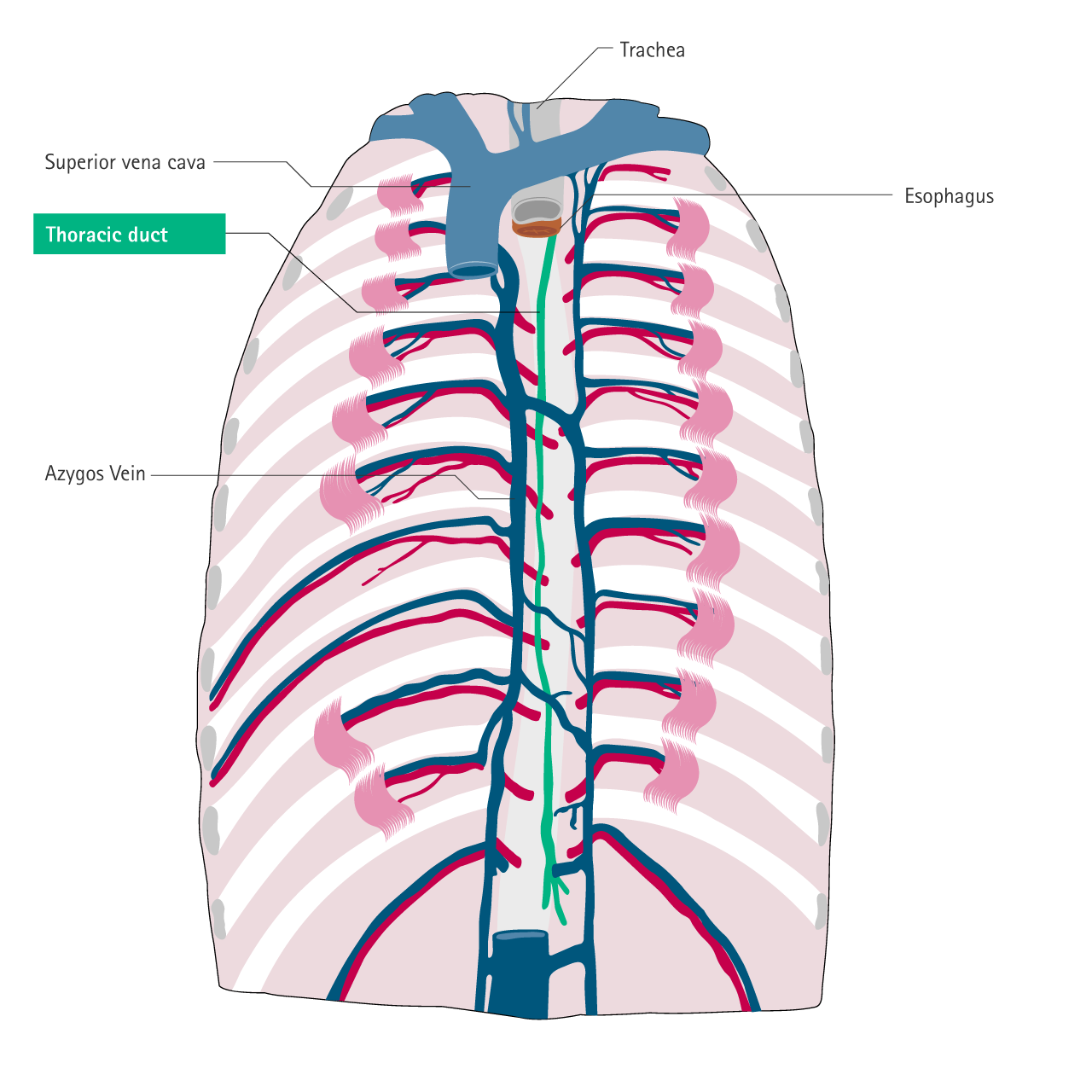
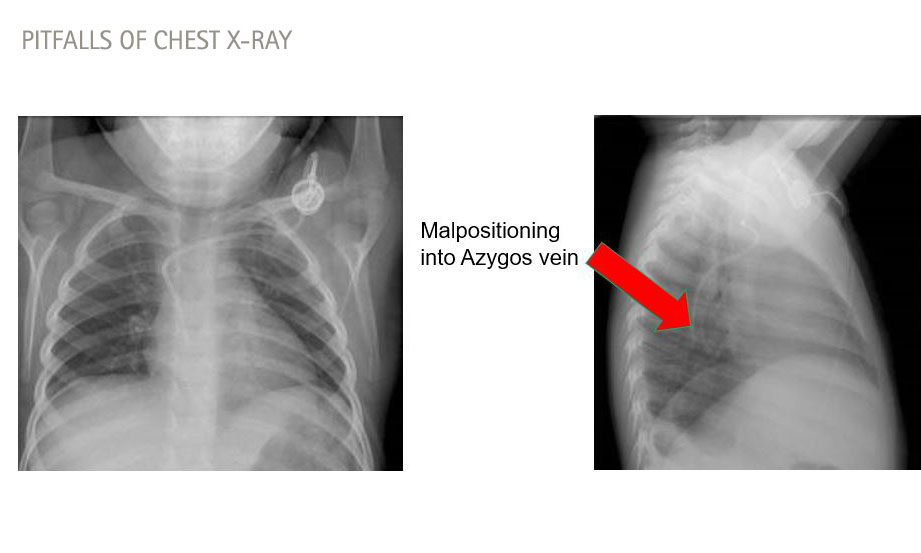
- Complex or abnormal anatomy (e.g. dilated azygos vein, high CVP, blocked SVC, IVC, persistent left superior vena cava)
Physician/Hospital factors
- Staff lack of knowledge, training and experience
- Under time pressure, stressful environment
- Pinch off Syndrome
- Catheter dislocation (not correctly secured)
Product factors
- No navigation technique available (Ultrasound, ECG)
- Inappropriate catheter size or length
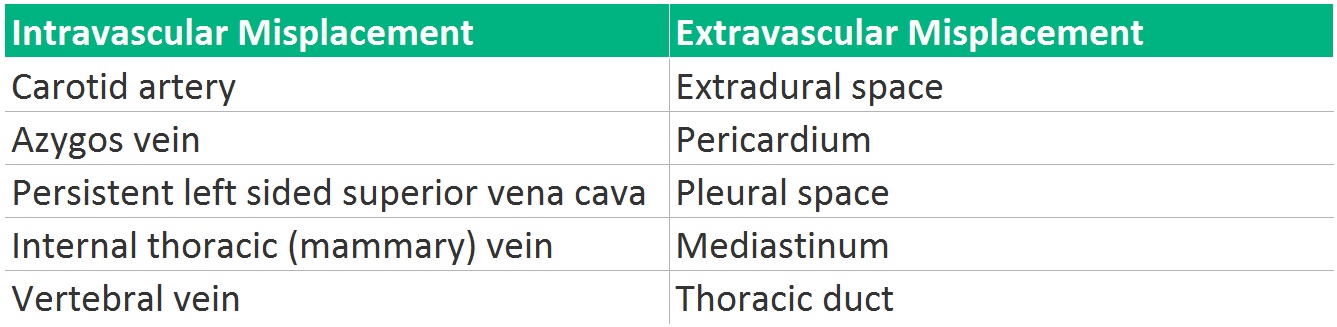
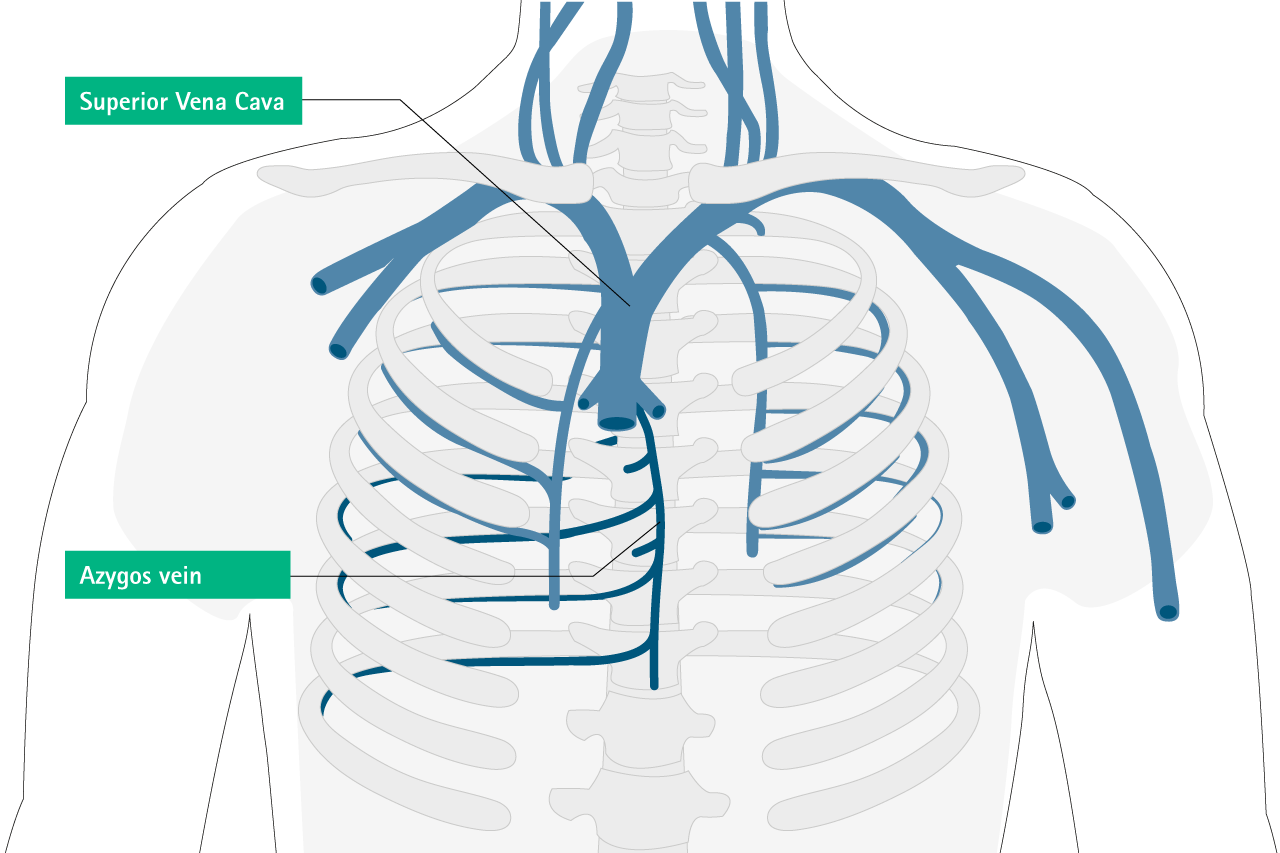
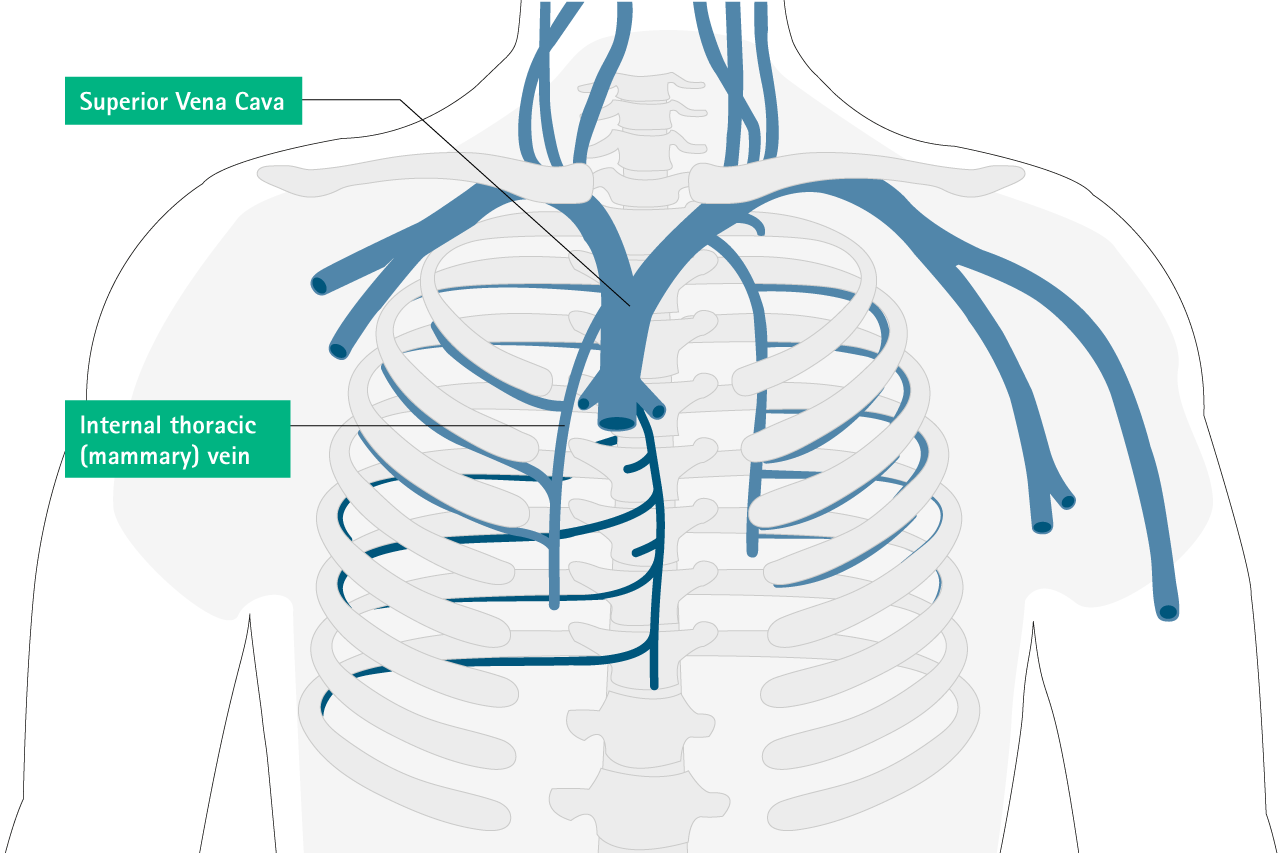
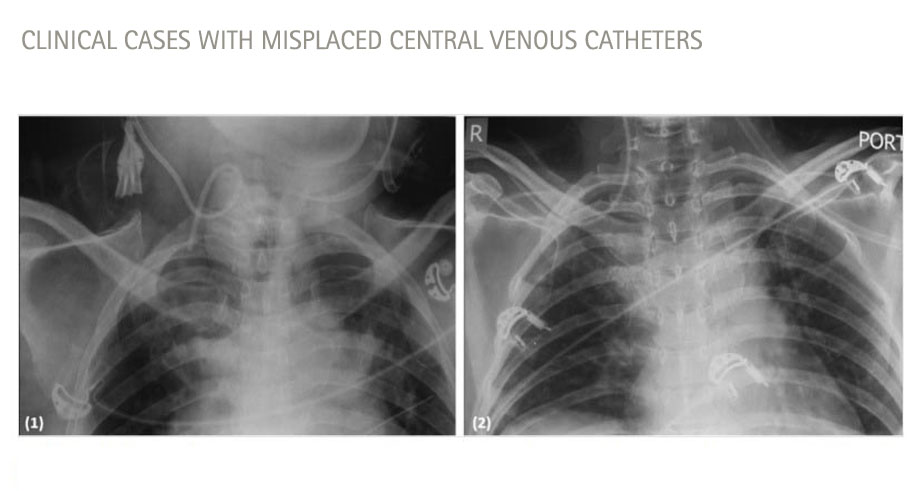
Type and Position of Catheter Misplacement12
Intravascular Misplacement
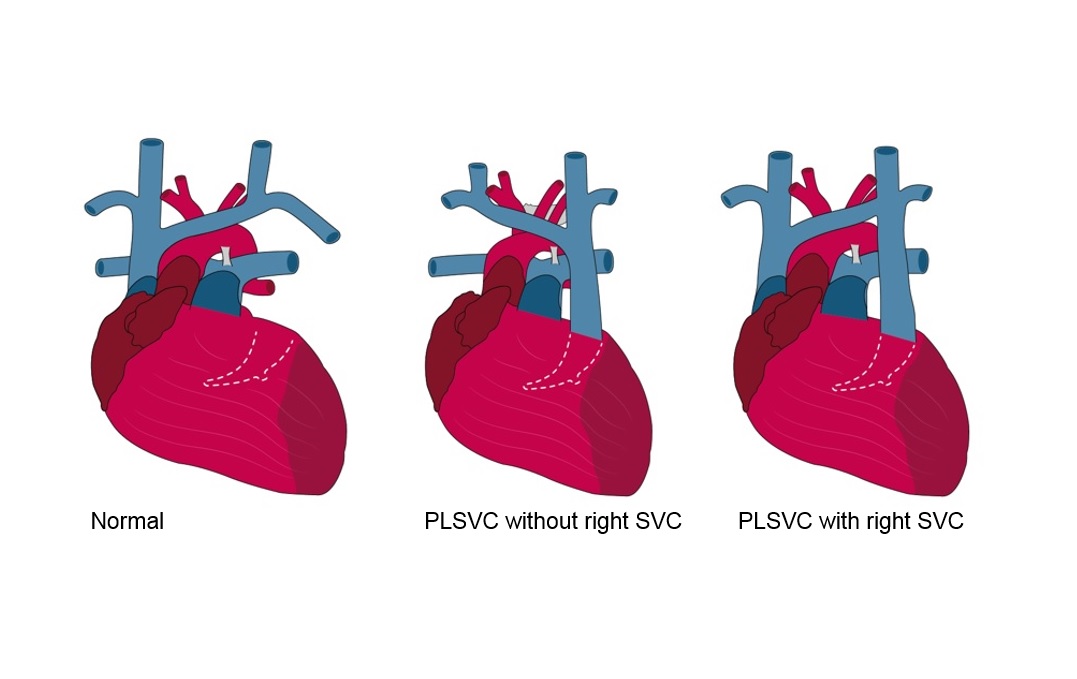
Persistent left sided Superior Vena Cava
Persistent left superior vena cava is a rare but important congenital vascular anomaly. present in 0.3 to 0.5% of individuals in the general population with a normal heart, and 4.5% in individuals with congenital heart diseases. In undiagnosed cases with PLSVC, placement of CVC can result in malpositioning.
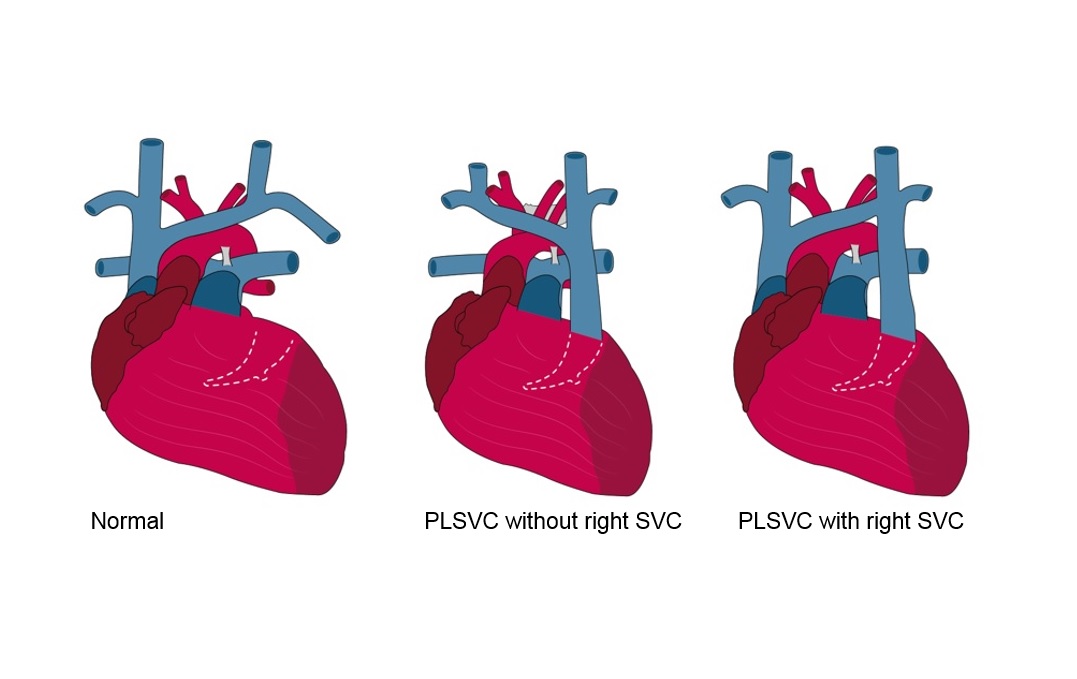
Persistent left sided Superior Vena Cava
Persistent left superior vena cava is a rare but important congenital vascular anomaly. present in 0.3 to 0.5% of individuals in the general population with a normal heart, and 4.5% in individuals with congenital heart diseases. In undiagnosed cases with PLSVC, placement of CVC can result in malpositioning.
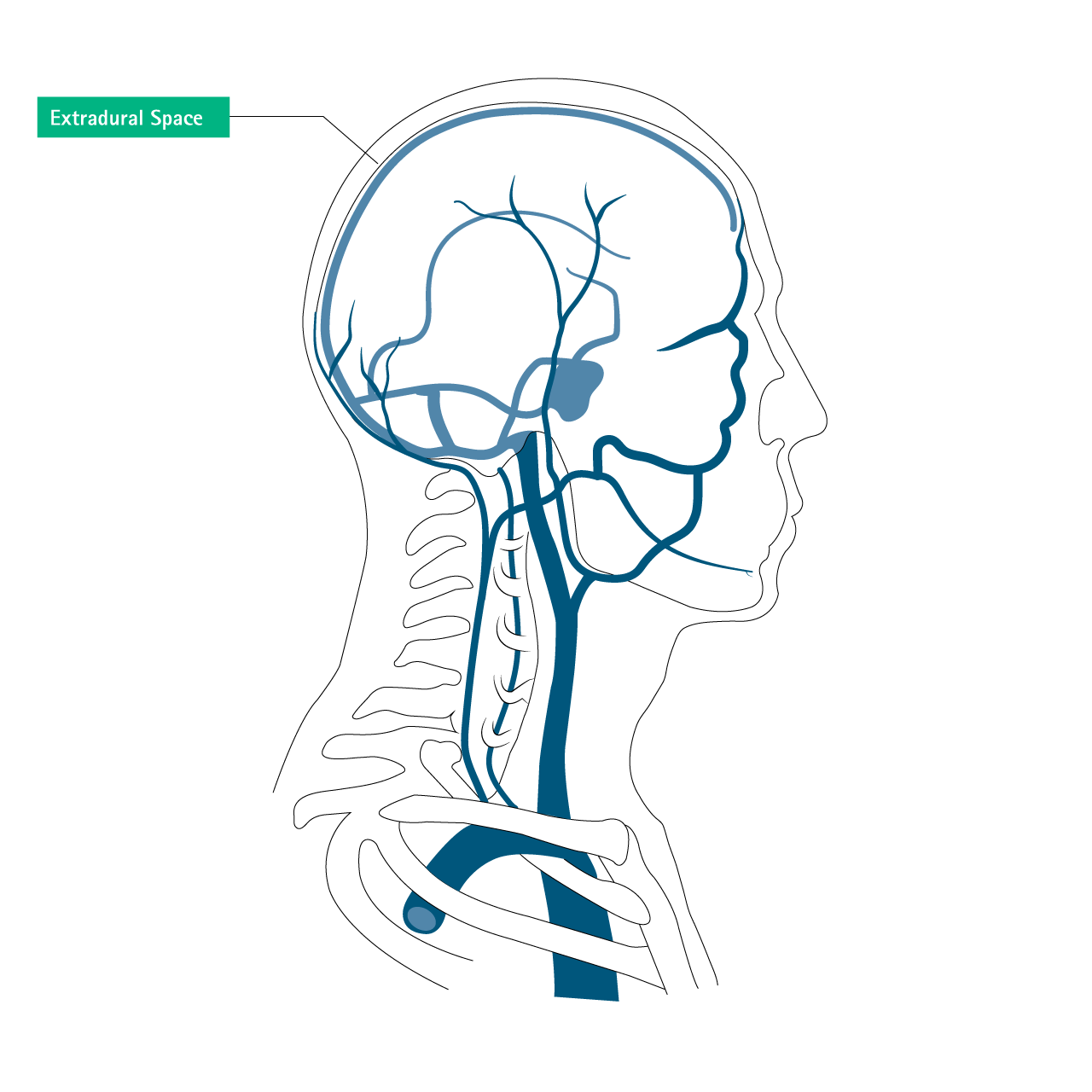
Extravascular Misplacement
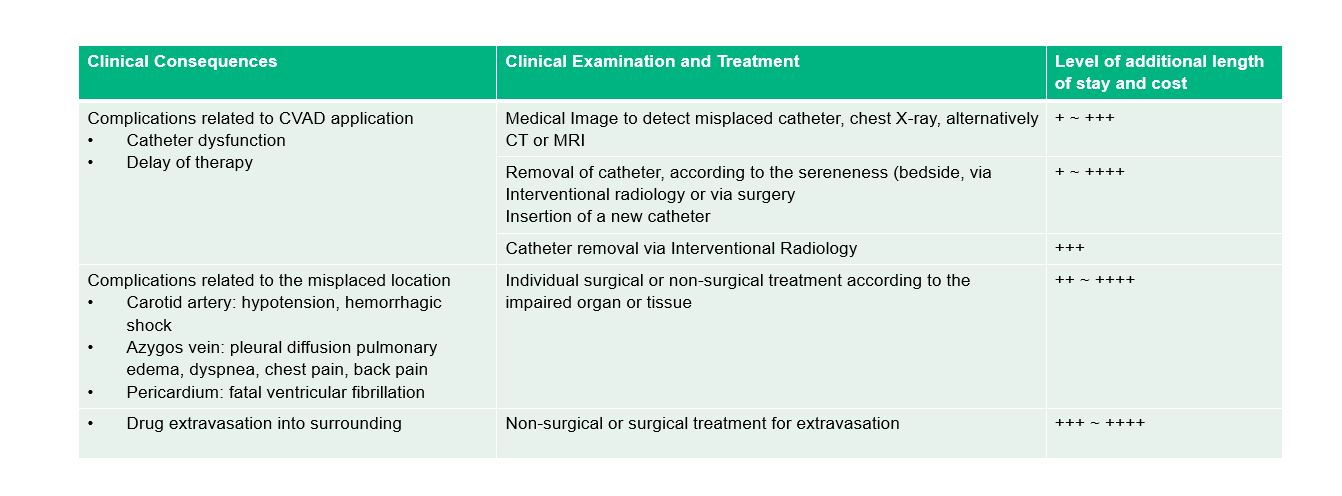
Health Consequences due to misplaced CVADs
Consequences related to CVC application
- Catheter dysfunction
- Delay of critical therapy (e.g. vasopressors, chemotherapy)
Consequences related to Access Ports application
- Pinch off Syndrom
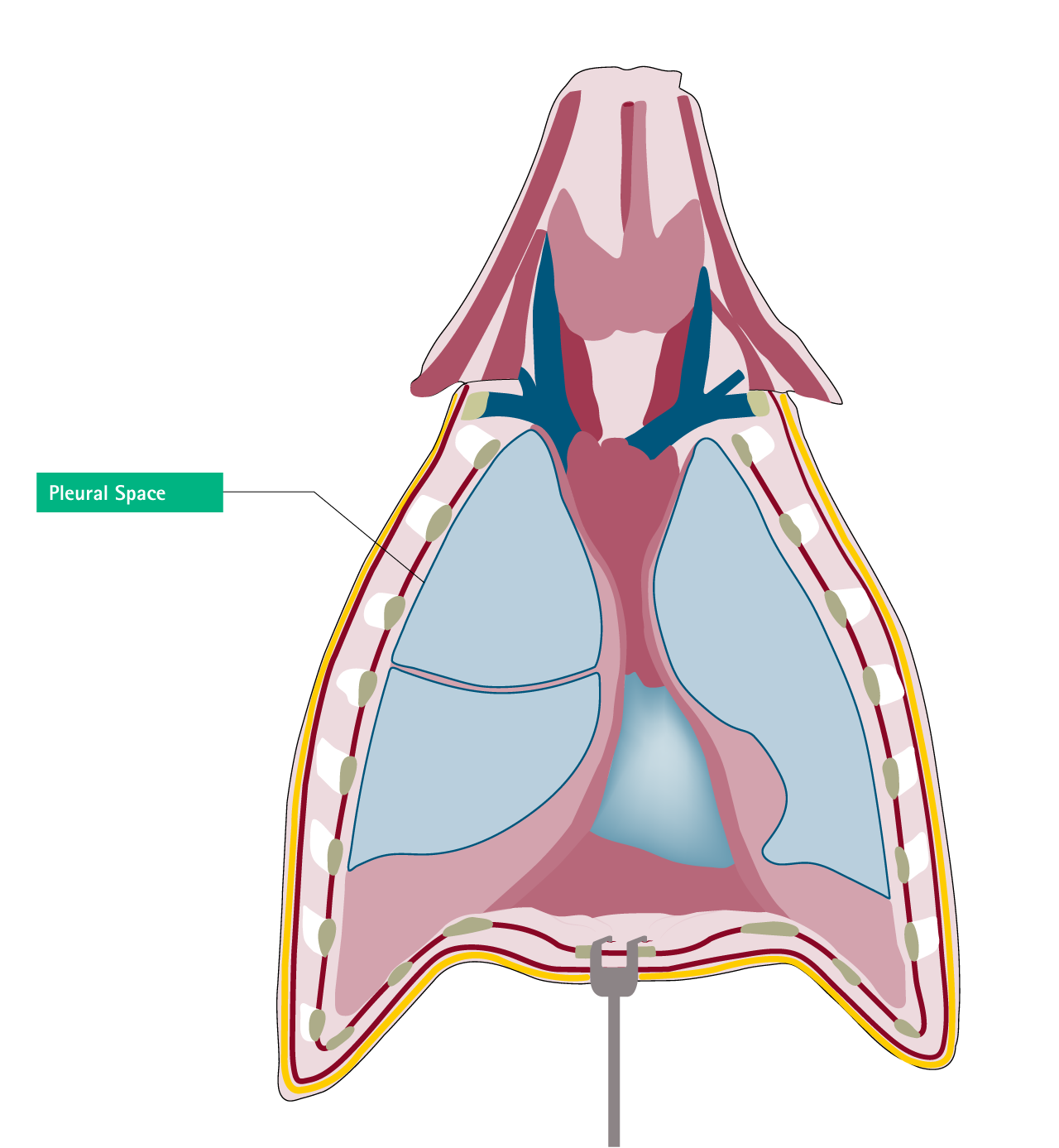
- Pneumothorax
- Hemothorax
- Air embolism
- Accidential arterial puncture
Complications related to PICC application
- Accidential arterial puncture
- Hematoma
- Difficulties in finding the vein
Complications related to the misplaced location12
- Carotid Artery: Hypotension, hemorrhagic shock
- Azygos Vein: Pleural diffusion pulmonary edema, dyspnea, chest pain, back pain
- Pericardium: Fatal ventricular fibrillation
- Drug extravasation into surrounding -> tissue necrosis, organ dysfunction
Financial Consequences for misplacement CVADs
Estimated level of costs (time, material, and personnel) related to diagnostic procedures, delay of therapy and required management for misplaced CVADs
Preventive Strategies
Selecting the proper vessel
- Incidence of malpositioning is higher in the left thoracic venous system than in the right side
- The right side of the circulation should be considered of first preference for CVC insertion unless those insertion sites are contraindicated.
- Use ultrasound for selecting the proper vessel for insertion
Select/trim the correct catheter length according to the insertion site and patient’s condition
Use the different technique correctly to implant TIVADs and PICCs (Seldinger, OTW, surgical cutdown)16
Use of Valve Needles to access the vein for central venous catheters: Save time/no disconnection needed.
Secure the CVADs sufficiently
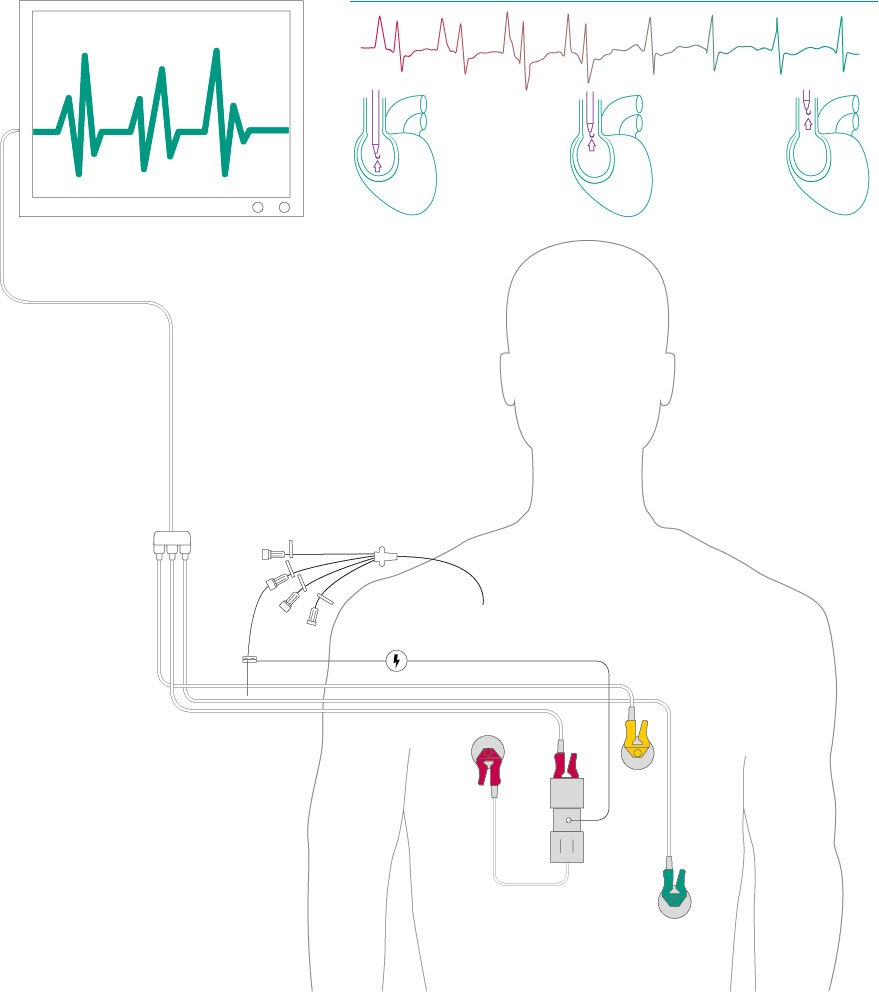
Select a proper device to guide insertion and confirm tip position
- Ultrasound guidance
- Intraatrial ECG
- Chest X-Ray17
- Other supporting methods/techniques: electromagnetic, manometry (needle and catheter, pressure waveform analysis, blood gas analysis8-12
Use of Valve Needle for venous access: save time/no disconnection needed
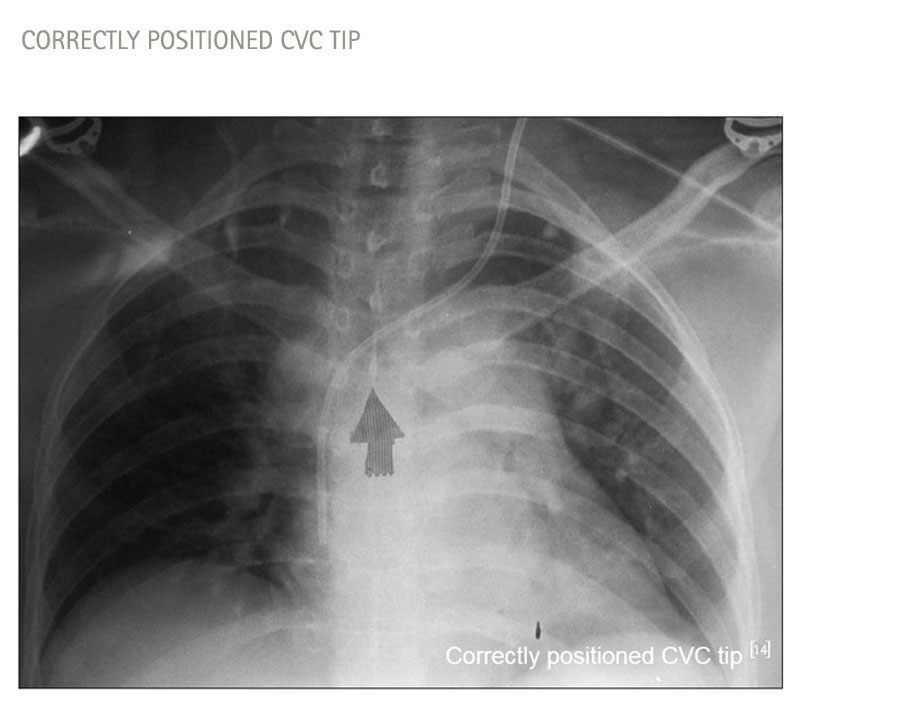
Verification of Catheter Position with Medical Imaging
X-Ray
- Plain Chest X-Ray is most commonly used to confirm catheter position within the chest and to detect pneumothorax, haemothorax or effusions after CVC placement
- Due to the 2D projection the close anatomical proximity of major arteries, veins, and pleura in the neck and chest causes difficulties and it is not possible to reliably state whether the distal section of the catheter is in an artery, vein, pleura, or mediastinum in the chest
- The intraatrial (intravascular) ECG technique can be used to confirm CVAD tip position during or after CVAD placement 9,10,18
- Intracavity (Intravascular or intraatrial) ECG tip positioning method with Certodyn and Alphacard is accurate, safe, feasible in all adult and paediatric patients9,18
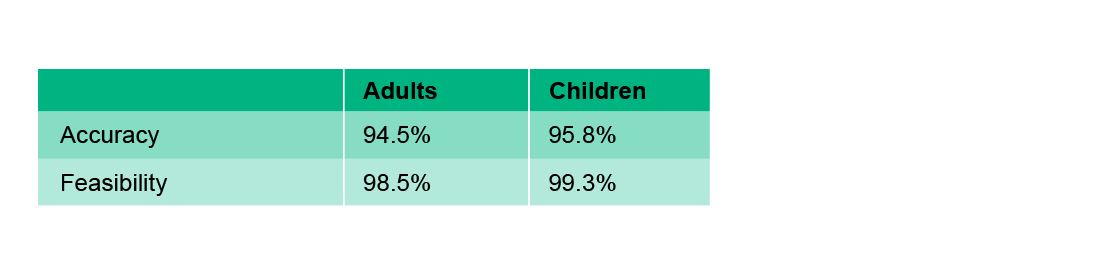
- ECG Method: Accuracy and Feasibility compared with Radiography9,18
- Ultrasound can be used to assess the jugular, femoral, axillary, and arm veins to aid insertion of a CVC, but is of limited value in confirming tip position in the SVC
- Transesophageal ultrasound (TEE) can be used if available to directly image the SVC, but this has practical limitations due to availability and operator training
- Transthoracic echo (TTE) can identify catheters in the RA, particularly with the injection of bubble contrast, but is not used in routine practice8-11
Highlight Safety Products
Central Venous Catheters (CVC) Devices
Scientific Evidence
References
1 Ho C, Spry C. Central Venous Access Devices (CVADs) and Peripherally Inserted Central Catheters (PICCs) for Adult and Pediatric Patients: A Review of Clinical Effectiveness and Safety 2017.
2 M. Pittiruti, A. La Greca, G. Scoppettuolo. The Electrocardiographic Method for Positioning the Tip of Central Venous Catheters. undefined 2011.
3 Graham AS, Ozment C, Tegtmeyer K, Lai S, Braner DAV. Videos in clinical medicine. Central venous catheterization. N Engl J Med 2007; 356: e21. https://doi.org/10.1056/NEJMvcm055053.
4 Gibson F, Bodenham A. Misplaced central venous catheters: applied anatomy and practical management. British journal of anaesthesia 2013; 110: 333–46. https://doi.org/10.1093/bja/aes497.
5 Schutz JCL, Patel AA, Clark TWI, et al. Relationship between chest port catheter tip position and port malfunction after interventional radiologic placement. Journal of vascular and interventional radiology: JVIR 2004; 15: 581–87. https://doi.org/10.1097/01.rvi.0000127890.47187.91.
6 Caers J, Fontaine C, Vinh-Hung V, et al. Catheter tip position as a risk factor for thrombosis associated with the use of subcutaneous infusion ports. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer 2005; 13: 325–31. https://doi.org/10.1007/s00520-004-0723-1.
7 Kornbau C, Lee KC, Hughes GD, Firstenberg MS. Central line complications. International Journal of Critical Illness and Injury Science 2015; 5: 170–78. https://doi.org/10.4103/2229-5151.164940.
8 McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med 2003; 348: 1123–33. https://doi.org/10.1056/NEJMra011883.
9 Rossetti F, Pittiruti M, Lamperti M, Graziano U, Celentano D, Capozzoli G. The intracavitary ECG method for positioning the tip of central venous access devices in pediatric patients: results of an Italian multicenter study. The journal of vascular access 2015; 16: 137–43. https://doi.org/10.5301/jva.5000281.
10 Pelagatti C, Villa G, Casini A, Chelazzi C, Gaudio AR de. Endovascular electrocardiography to guide placement of totally implantable central venous catheters in oncologic patients. The journal of vascular access 2011; 12: 348–53. https://doi.org/10.5301/JVA.2011.8380.
11 Parienti J-J, Mongardon N, Mégarbane B, et al. Intravascular Complications of Central Venous Catheterization by Insertion Site. N Engl J Med 2015; 373: 1220–29. https://doi.org/10.1056/NEJMoa1500964.
12 Wang L, Liu Z-S, Wang C-A. Malposition of Central Venous Catheter: Presentation and Management. Chin Med J (Engl) 2016; 129: 227–34. https://doi.org/10.4103/0366-6999.173525.
13 Smit JM, Raadsen R, Blans MJ, Petjak M, van de Ven PM, Tuinman PR. Bedside ultrasound to detect central venous catheter misplacement and associated iatrogenic complications: a systematic review and meta-analysis. Critical care (London, England) 2018; 22: 65. https://doi.org/10.1186/s13054-018-1989-x.
14 Roldan CJ, Paniagua L. Central Venous Catheter Intravascular Malpositioning: Causes, Prevention, Diagnosis, and Correction. West J Emerg Med 2015; 16: 658–64. https://doi.org/10.5811/westjem.2015.7.26248.
15 Fletcher SJ, Bodenham AR. Safe placement of central venous catheters: where should the tip of the catheter lie? British journal of anaesthesia 2000; 85: 188–91. https://doi.org/10.1093/bja/85.2.188.
16 Stas M, Mulier S, Pattyn P, Vijgen J, Wever I de. Peroperative intravasal electrographic control of catheter tip position in access ports placed by venous cut-down technique. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 2001; 27: 316–20. https://doi.org/10.1053/ejso.2000.1047.
17 Venugopal AN, Koshy RC, Koshy SM. Role of chest X-ray in citing central venous catheter tip: A few case reports with a brief review of the literature. Journal of anaesthesiology, clinical pharmacology 2013; 29: 397–400. https://doi.org/10.4103/0970-9185.117114.
18 Pittiruti M, Bertollo D, Briglia E, et al. The intracavitary ECG method for positioning the tip of central venous catheters: results of an Italian multicenter study. The journal of vascular access 2012; 13: 357–65. https://doi.org/10.5301/JVA.2012.9020.