Definition: What is malnutrition?
The term malnutrition can be defined as “a state resulting from lack of intake or uptake of nutrition that leads to altered body composition (decreased fat-free mass) and body cell mass, leading to diminished physical and mental function, and impaired clinical outcome from disease”.1 Malnutrition is not only weight loss; it is also seen as a combination of poor appetite and unintended weight loss over time.
Potential risk factors
Selection of potential risk factors for malnutrition
- Food supply
- Accelerated catabolism because of trauma and inflammatory diseases2
- Age3
- Living alone3
- Polypharmacy3
- Malignant diseases like cancer3,4
- Metabolic derangements (host- or tumor-derived)5
Not only physical conditions like malignant diseases play a role in developing malnutrition, but also social factors like aging (> 60 years), living alone, polypharmacy and many more contribute to the state.3
Besides of food supply, accelerated catabolism caused by trauma and inflammatory diseases2 [disease-related malnutrition (DRM1)] is another risk factor.
Patients with malignant diseases like cancer show a high risk of malnutrition.3,4 But unlike simple malnutrition, the negative energy balance and skeletal muscle loss observed in cancer patients is driven by a combination of reduced food intake and metabolic derangements, which may be host- or tumor-derived.5
One of these is the inflammatory response in cancer patients, causing anorexia and tissue breakdown, and leading to significant loss of body weight, alterations in body composition, and declining physical function.5
How to diagnose?
International guidelines such as ESPEN strongly recommend nutritional screening and assessment tools for diagnosing malnutrition.5 There are several screening tools available. They should be valid, reliable and practical as well as fast, simple and intuitive.6
After evaluating the answers resulting from the screening tools, a more detailed and comprehensive baseline nutritional assessment of the patient should follow. This assessment clarifies the nutritional diagnosis and establishes the severity of malnutrition.
Finally, based on the nutritional assessment, an appropriate nutrition intervention should be implemented.7
Diagnostic criteria
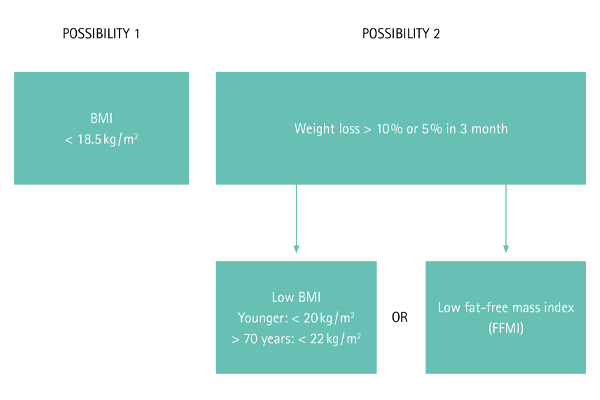
For the general population, the diagnostic criteria for malnutrition according ESPEN is either a reduced BMI < 18.5 kg / m2 in accordance with the underweight definition provided by WHO or combined weight loss and reduced BMI (age dependent cut-offs) or reduced gender-dependent fat-free mass index (FFMI).8
However, the ESPEN and ASPEN recommend screening tools like NRS (Nutritional Risk Screening), MUST (Malnutrition Universal Screening Tool), MNA (Minimal Nutritional Assessment), SGA (Subjective Global Assessment), and PG-SGA (Patient-Generated Subjective Global Assessment) to diagnose malnutrition in cancer patients.5,9 Low BMI in combination with weight loss is also found in these screening tools.
Nutrition intervention
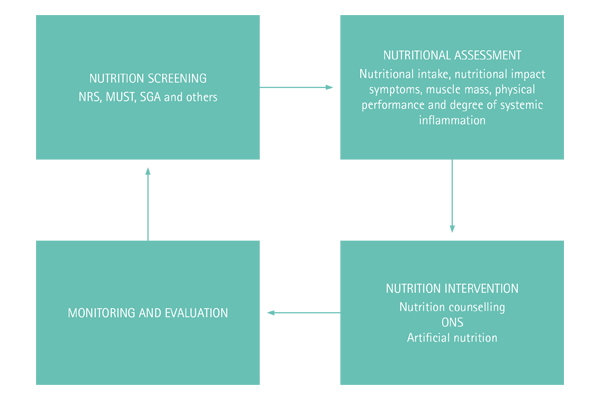
Nutrition intervention can be nutrition counselling with or without artificial nutrition (enteral or parenteral nutrition) and should be monitored for evaluation.1 The standardized process from screening to nutrition intervention and evaluation is called the nutrition care process (Fig. 1).5,7
References
1 Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49-64.
2 van Bokhorst-de van der Schueren MA, Soeters P, Reijven PLM, Allison SP, Kondrup J. Definition of malnutrition. In: Sobotka L, editor. ESPEN Book: Basics in Clinical Nutrition. 4 th ed: GALEN; 2011. p. 21-2.
3 Pirlich M, Schutz T, Kemps M, Luhman N, Minko N, Lubke HJ, et al. Social risk factors for hospital malnutrition. Nutrition. 2005;21(3):295-300.
4 Pirlich M, Schutz T, Norman K, Gastell S, Lubke HJ, Bischoff SC, et al. The German hospital malnutrition study. Clin Nutr. 2006;25(4):563-72.
5 Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36(1):11-48.
6 Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22(4):415-21.
7 Gibson RS. Principles of Nutritional Assessment. 2 nd ed: OXFORD University press; 2005.
8 Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition - An ESPEN Consensus Statement. Clin Nutr. 2015;34(3):335-40.
9 Mueller C, Compher C, Ellen DM. A.S.P.E.N. clinical guidelines: Nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enteral Nutr. 2011;35(1):16-24.