Sharps Injury
Sharp Injuries are skin penetrating stab wounds caused by sharp instruments and accidents in a medical setting. These instruments include needles, lancets, scalpels and broken glass.1,2
Needlestick Injuries (NSIs) are defined as an accidental skin penetrating stab wound caused by hollow-bore needles such as hypodermic needles, blood-collection needles, IV catheter stylets, and needles used to connect parts of IV delivery system.2,3
Did you Know?
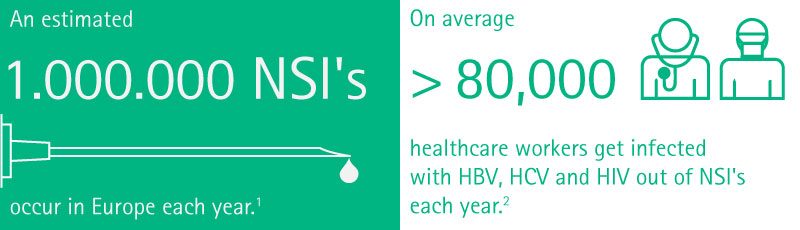
(1) Himmelreich, H., et al.The Management of Needlestick Injuries. Dtsch Arztebl Int. 2013 Feb; 110(5): 61–67.
(2) Prüss-Ustün A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005 Dec;48(6):482-90.
Causes
In general, needlestick injuries (NSIs) are caused by simple and preventable mistakes in handling sharp medical devices.1,7
The Centers for Disease Control and Prevention (CDC) summarize the most common causes1,7
- lack of personal protective equipment, safety devices, and sharps disposal containers
- lack of procedures for sharps injury reporting
- lack of awareness with occupational hazards
- insufficiently trained staff
- limited access to sharps disposal containers
- shortage of staff
- recapping needles after use
- passing sharp instruments from hand-to-hand in the operating suite
- failure to use sharps disposal containers immediately after use
- unpredictable medical incidents
- unexpected patient reactions.
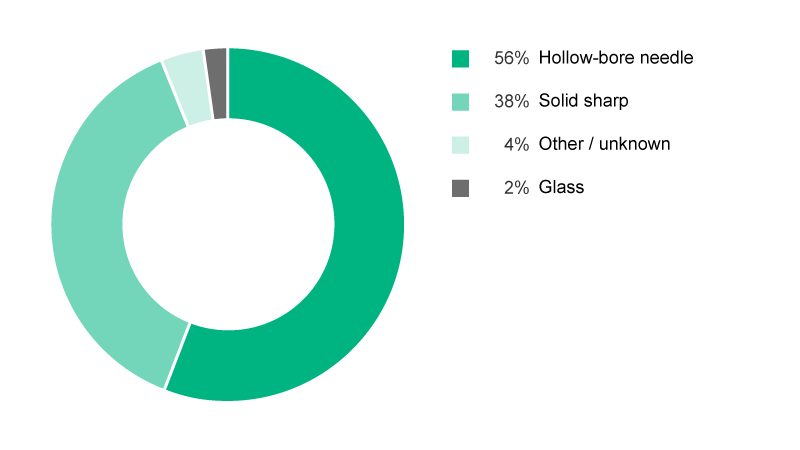
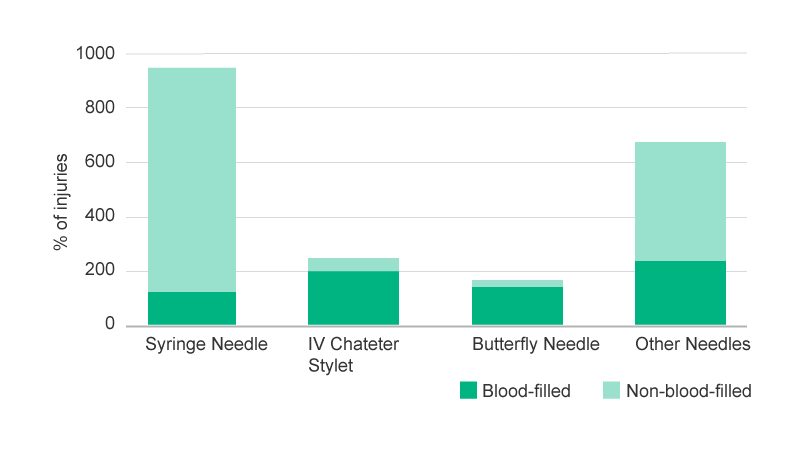
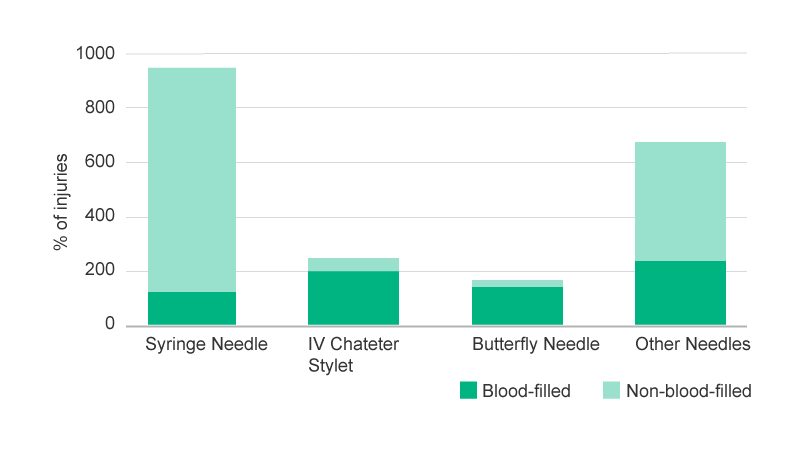
Percutaneous injuries
Percutaneous injuries represent the most dangerous situation for HCWs where safety products and measures haven’t already been established. Percutaneous injuries may be caused by objects like needles, surgical instruments or glass.7 Nearly 80% of all percutaneous sharps injuries are caused by a needlestick, with 56% attributed to hollow-bore needles (See Figure 1).1
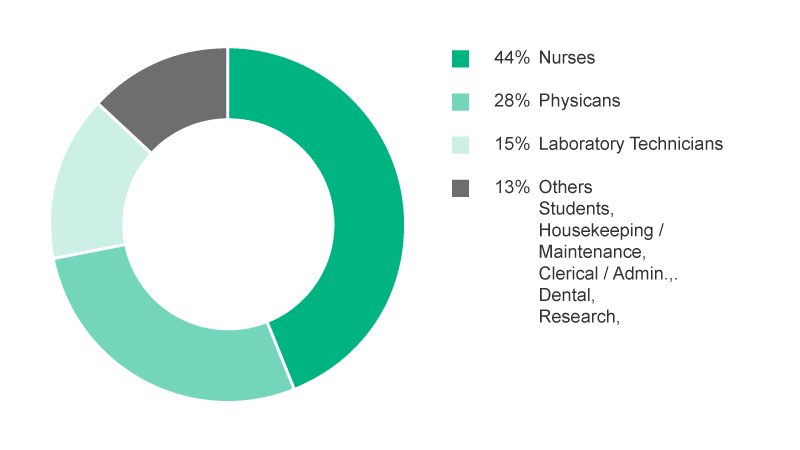
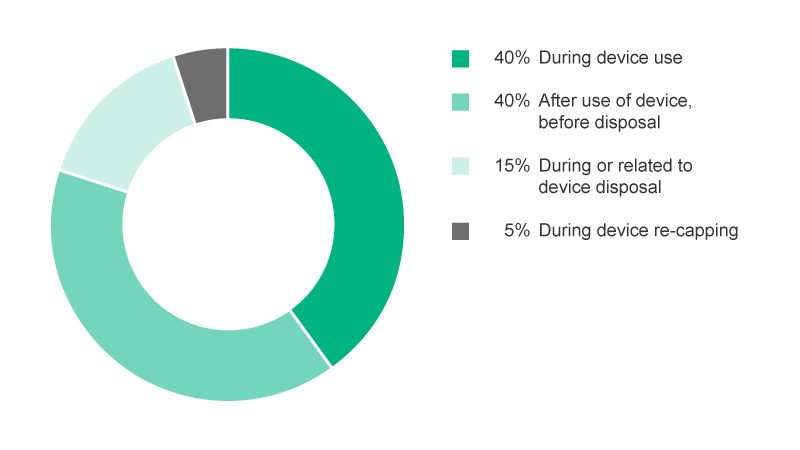
Syringe needles, IV catheter stylets, and Butterfly needles represent nearly 65% of all injuries from hollow-bore needles and are considered high-risk because they involve blood-filled needles. Nearly every 2nd hollow-bore needlestick also endangers the HCW to the risk of a blood exposure (See Figure 2).10 Additionally physicians and laboratory staff had an explicit risk of NSIs with contaminated hollow-bore needles.1,6 In addition to HCWs directly working with medical devices, house keeping and laundry personnel are also susceptible to the hazardous consequences of NSIs (See Figure 3).1,6
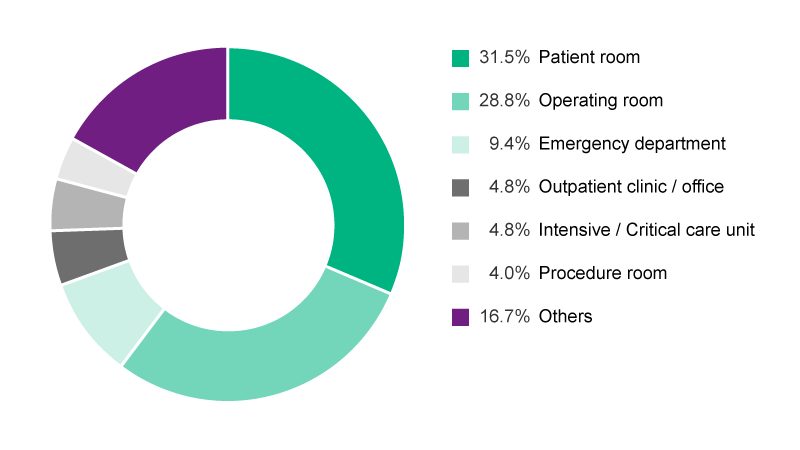
It is known, that most exposures occur within the patient room, followed by operating room and the emergency department (See Figure 5).8 Studies show an increased risk of injuries with rushing, anger, distraction, and multiple attempts to complete a procedure. Additional factors with a negative impact on safe handling were healthcare worker (HCW) fatigue, uncooperative patients, or teams affected by staff shortage.9,10
Incidence rate
The availability of actual figures regarding the incidence rates of needlestick injuries (NSIs) is insufficient and limited in general, especially for national and global figures. Two major factors are responsible for this situation:
- data is non-comprehensive due to a lack of surveillance and reporting systems in the concerned healthcare facilities.6
- the second factor is related to a prevalent and persisting underreporting of incidences, which has been demonstrated by numerous studies.8 As an example, Wicker published results demonstrating that only 28.7% of injured healthcare workers (HCWs) reported the NSI, 50.4% did not report the NSI and 20.9% only reported occasionally or gave no response in the surveillance questionnaire.3
In the U.S. an extensive survey documented an underreporting of 58%.13 Other studies exposed the severity of underreporting of needlesticks with estimates higher than 90%.14 Some principal reasons for not reporting were time constraints, perception that the percutaneous injury did not represent a significant exposure, lack of knowledge about the reporting mechanism and concern about confidentiality and professional discrimination.12
Health Consequences
The main concern regarding a needlestick injury (NSI) is not characterized by the trauma itself, but by the percutaneous exposure to a patient’s blood and body fluids (BBF) which may carry infectious disease.2,11
At least 20 different pathogens involving viruses, bacteria and fungi can be transmitted to healthcare workers (HCWs) through NSIs.1,7 The likelihood of developing a disease after a NSI depends on various independent factors: pathogen concentration in the BBF, depth of the wound, blood volume, amount of pathogens transmitted and the infection phase of the pathogen carrier. The seroconversion rate and availability of vaccinations or post exposure prophylaxis (PEP) treatments also play a critical role, as infected HCWs face the consequences of developing acute and chronic diseases and even the probability of death.2,12
Due to clinical severity and health complications, the most debilitating diseases associated with NSIs are the blood-borne pathogens HBV, HCV and HIV (See Fig. 6).
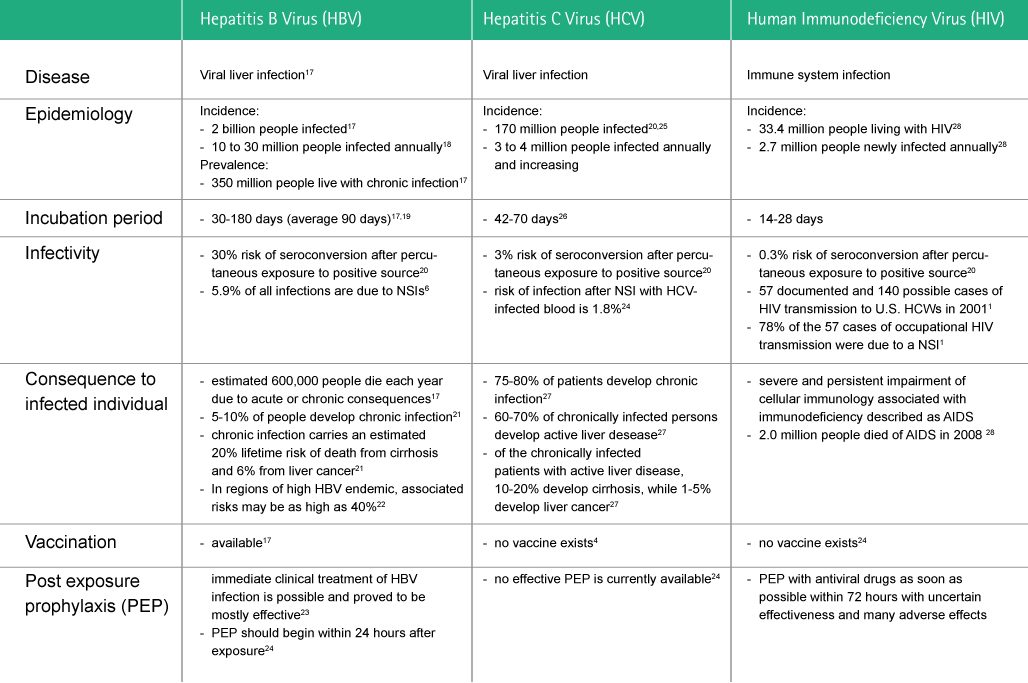
Fig. 6: Viruses with the highest risks associated with their transmission after sharp and needlestick injuries.
Financial Consequences
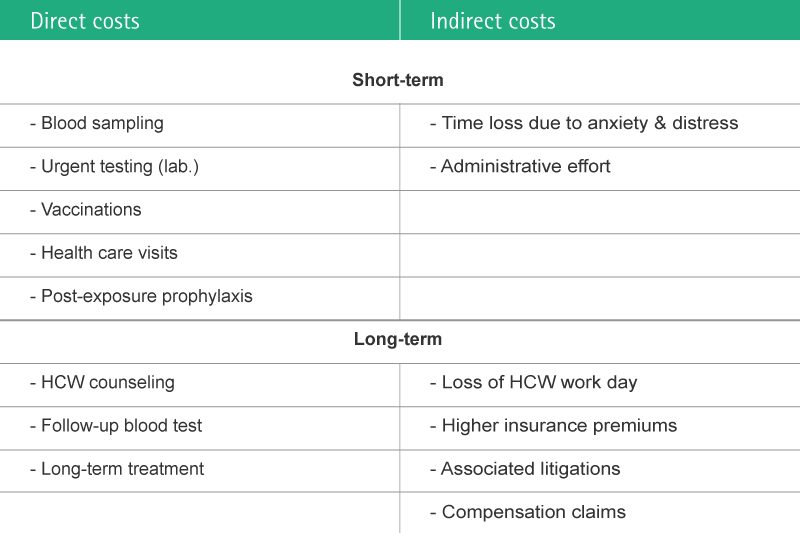
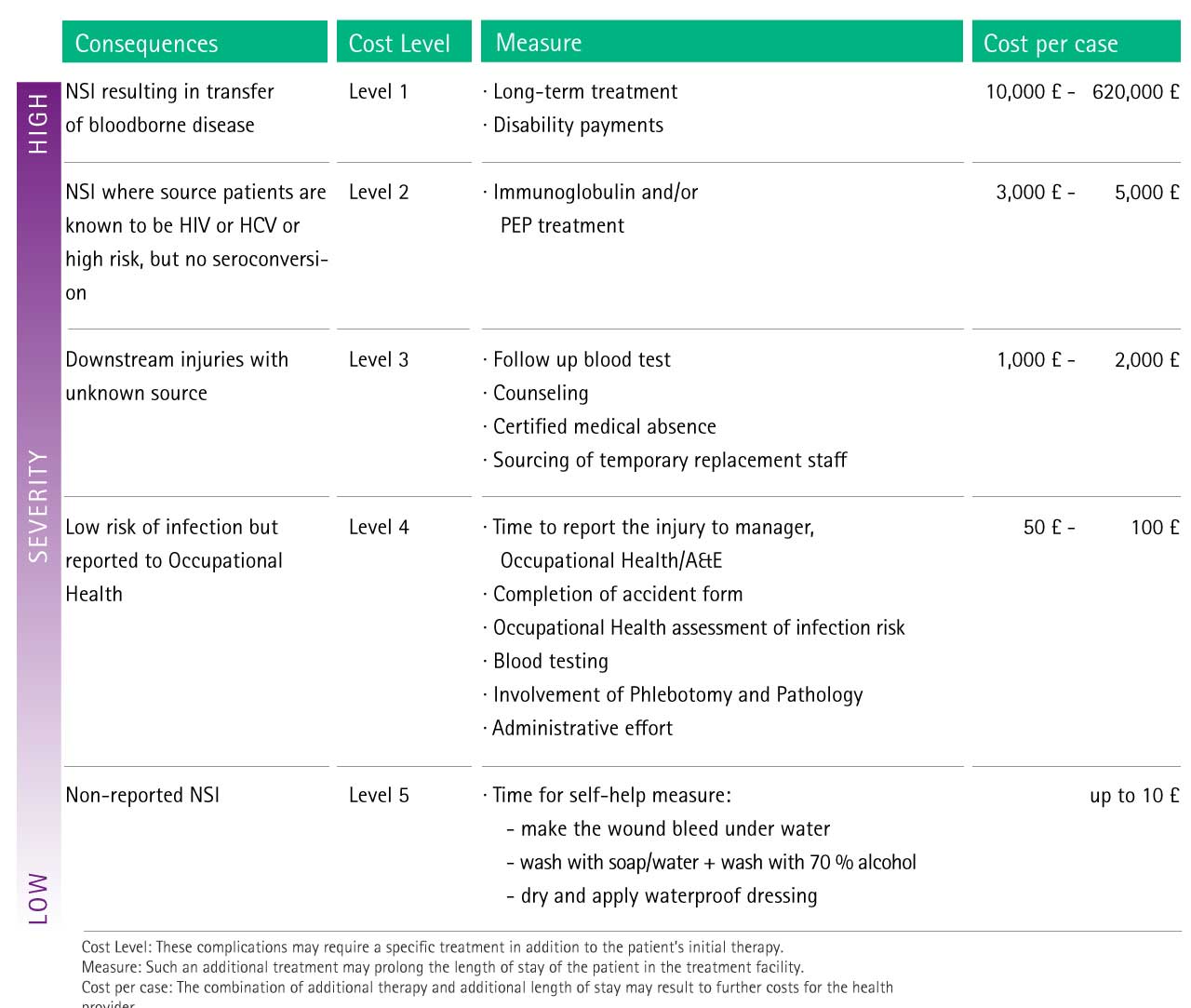
NSIs cause various direct and indirect costs due to their severe nature (See Fig. 7).
- Direct costs, such as follow-up diagnosis and medical treatments, are often a consequence of recommended procedures, showing therefore a more prominent impact to the healthcare facility.
- Indirect costs after a NSI must also be considered as important, because of staff retention, compensations for lost employment and damages, insurance premiums and future litigations (See Fig. 7). Furthermore, even a non-transmitted disease can produce emotional trauma and distress, resulting in personal counseling and productivity lost.8
Potential Risk Associated Cost
Various studies have estimated the financial impact of NSIs. As an example of short-term direct costs, Hatcher described that a single NSI would cost the healthcare facility $ 2,234 to $ 3,832.20
In the case of a transferred blood-borne disease after a NSI, the overall long-term financial cost has been calculated to be as high as 922,000 €.19
The Fig. 8 below shows an estimation of possible additional costs as a consequence of complications caused by sharps injury.
Preventive Strategies
The effective prevention of needlestick injuries (NSIs) to avoid the exposure to blood or body fluids (BBF) requires a comprehensive approach combining various strategies and actions4,9,11,17
- continuous education in safe use and disposal of sharp devices
- mandatory reporting of all sharps and NSIs
- use of needle-free systems where possible
- use of safety devices
- suitable access to and correct use of sharps containers
- immediate disposal of sharps into appropriate containers
- frequent collection and proper disposal of sharps containers
- ban recapping of needles
- elimination of unnecessary injections.
Training and education
A general training and educational program on universal precautions and proper use of sharp devices must be established in a hospital. This has to include not only the safe application of hollow-bore needles, but also their disposal, the adaptation of safe work practices and the reporting of NSIs.4,9,11,17
As an example of an effective reduction of injuries, the implementation of point-of-use sharps containers lowered recapping-associated needlesticks from 23% of all needlesticks to only 5% (See Figure 9).5
Needle protective devices
Experience shows that continuous reinforcement of educational strategies alone may be insufficient to sustain a reduction of NSIs.18
Therefore the prevention of NSIs has to be enforced by the use of needle protective devices. The introduction of safety devices instead of non-protected conventional devices can achieve a significant reduction of the risk of NSIs.11
The effectiveness of safety devices varies between the device type and departments within the healthcare setting. Basically, safety devices have been shown to reduce NSIs by 22% to 100%. Consequently, in some areas the transmission of pathogens from percutaneous injuries could be nearly eliminated (See Fig. 10).8
Safer sharp devices
Under evidence-based criteria, the clinical data are incomplete. For the Cochrane database, a systematic review found very low quality evidence that needle protective devices result in a decrease of NSI compared with non-protected conventional devices.9 A second systematic review concluded that the use of safer sharps devices is considered to improve safety and reduce the incidence of healthcare worker needlestick injuries. However, their use is not regarded as a complete solution to reducing sharps related injuries amongst health care workers. Furthermore, safer sharps devices should be introduced alongside appropriate educational programmes.18
Highlight Safety Products
Scientific Evidence
1 Centers for Disease Control and Prevention. Workbook for Designing, Implementing and Evaluating a Sharps Injury Prevention Program. Update 2015
2 Riddell A, Kennedy I2, Tong CY3. Management of sharps injuries in the healthcare setting. BMJ. 2015 Jul 29;351:h3733. doi: 10.1136/bmj.h3733
3 Wicker S, Stirn AV, Rabenau HF, von Gierke L, Wutzler S, Stephan C. Needlestick injuries: causes, preventability and psychological impact. Infection. 2014 Jun;42(3):549-52
4 Yang L, Mullan B. Reducing needle stick injuries in healthcare occupations: an integrative review of the literature. ISRN Nurs. 2011;2011:315432. doi: 10.5402/2011/315432
5 Jagger J, Bentley MB. Injuries from vascular access devices: high risk and preventable. Collaborative EPINet Surveillance Group. J Intraven Nurs. 1997 Nov-Dec;20(6 Suppl):S33-9
6 Rapiti E, Prüss-Üstün A, Hutin Y. Sharps injuries - Assessing the burden of disease from sharps injuries to health-care workers at national and local levels. Environmental Burden of Disease Series, No. 11. WHO 2005
7 National Institute for Occupational Safety and Health. NIOSH Alert: Preventing Needlestick Injuries in Health Care Settings. Centers for Disease Control and Prevention. (NIOSH). 2004
8 Perry J, Jagger J. Healthcare Worker Blood Exposure Risk: Correcting Some Outdated Statistics. Advances in Exposure Prevention. 2003;6(3)28-31
9 Lavoie MC, Verbeek JH, Pahwa M. Devices for preventing percutaneous exposure injuries caused by needles in healthcare personnel. Cochrane Database Syst Rev. 2014 Mar 9;3:CD009740
10 Fisman DN, Harris AD, Rubin M, Sorock GS, Mittleman MA. Fatigue increases the risk of injury from sharp devices in medical trainees: results from a case-crossover study. Infect Control Hosp Epidemiol. 2007 Jan;28(1):10-7
11 Higginson R, Parry A. Needlestick injuries and safety syringes: a review of the literature. Br J Nurs. 2013 Apr 25-May 8;22(8):S4, S6-8, S10
12 Hadaway L. Needlestick injuries, short peripheral catheters, and health care worker risks. J Infus Nurs. 2012 May-Jun;35(3):164-78
13 Alvarado F, Panlilio A, Cardo D, NaSH Surveillance Group. Percutaneous injury reporting in U.S. hospitals, 1998. In: Program and Abstracts of the 4th Decennial International Conference on Nosocomial and Healthcare-Associated Infections. Atlanta, GA: Centers for Disease Control and Prevention. Abstract P-S2-38 Trim JC, Elliott TSJ. A review of sharp injuries and preventative strategies. J Hosp Infect 2003;53:237-242 www.ncbi.nlm.nih.gov/pubmed/12660120
14 Trim JC, Adams D, Elliott TS. Healthcare workers' knowledge of inoculation injuries and glove use. Br J Nurs. 2003 Feb 27-Mar 12;12(4):215-21
15 Panlilio AL, Orelien JG, Srivastava PU, Jagger J, Cohn RD, Cardo DM; NaSH Surveillance Group; EPINet Data Sharing Network. Estimate of the annual number of percutaneous injuries among hospital-based healthcare workers in the United States, 1997-1998. Infect Control Hosp Epidemiol. 2004 Jul;25(7):556-62
16 Hofmann F, Kralj N, Beie M. Needle stick injuries in health care - frequency, causes und preventive strategies. Gesundheitswesen. 2002 May;64(5):259-66
17 De Carli G, Abiteboul D, Puro V. The importance of implementing safe sharps practices in the laboratory setting in Europe. Biochem Med (Zagreb). 2014 Feb 15;24(1):45-56
18 HSE. Health and Safety Executive. An evaluation of the efficacy of safer sharps devices. Systematic review. Prepared by the Health and Safety Laboratory for the Health and Safety Executive 2012
19 National Health Service for Scotland (NHS Scotland). Needlestick Injuries: Sharpen Your Awareness. Report of the Short Life Working Group on Needlestick Injuries in the NHS Scotland. Edinburgh: National Health Services for Scotland:2001. www.scotland.gov.uk/Publications/2001/05/9167/File-1
20 Hatcher IB. Reducing Sharps Injuries Among Health Care Workers: A Sharps Container Quality Improvement Project. Jt Comm J Qual Improv 2002;28(7):410-414 www.ncbi.nlm.nih.gov/pubmed/12101553
21 Tan L, Hawk JC, Sterling ML. Report of the Council Scientific Affairs: Preventing Needlestick Injuries in Health Care Settings. Arch Intern Med 2001;161(7):929-936 http://www.ncbi.nlm.nih.gov/pubmed/11295955
22 Himmelreich, H., et al.The Management of Needlestick Injuries. Dtsch Arztebl Int. 2013 Feb; 110(5): 61–67
23 Prüss-Ustün A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005 Dec;48(6):482-90