Goals of nutritional support
It is important to define the goals of nutritional therapy, realistic and proven by evidence.
Therapeutic goals for nutritional therapy in cancer patients according to international organizations could be:
- Maintain or improve nutritional status1
- Maintain or improve food intake1
- Mitigate metabolic derangements2
- Prevent and treat undernutrition / cachexia3
- Enhance compliance with anti-tumor treatments1,3
- Maintain skeletal muscle mass and physical performance1
- Control some adverse effects of anti-tumor therapies3
- Improve QoL1,3
Background information: recent studies showing status quo
There are several studies describing that many patients with malnutrition do not receive nutritional support.4,5
In a study from Spain, only a third of the patients at risk of malnutrition upon discharge had received any kind of nutritional support, with older cancer patients (> 70 years) receiving even less than younger cancer patients5 (see Fig. 1).
A 1-day prevalence survey in 154 French hospital wards showed that only 57.6% of malnourished and 28.4% of non-mal-nourished patients received nutritional support. Only 41.4% of patients stated that they had received nutrition counselling.4
In another previous study, 62% of malnourished patients received nutritional support (vs. 31.7% in the absence of malnutrition) including nutrition counselling alone (49.2%) or the use of oral supplementation or artificial nutrition (12.8%).6
A study from Australia reported that 35 % patients with malnutrition, significant weight loss and intake-limiting chemotherapy-induced nausea and vomiting (CINV) had no prior dietetic contact. The majority of those participants were overweight or obese and, therefore, possibly overlooked.7
It is not clear why not all malnourished patients get nutritional support, but it is probably due to a lack of awareness on the part of healthcare professionals or a lack of resources. Gyan et al. (2017) showed that malnutrition-associated symptoms were underestimated by physicians8 and this could be a reason nutrition counselling was not requested by them.
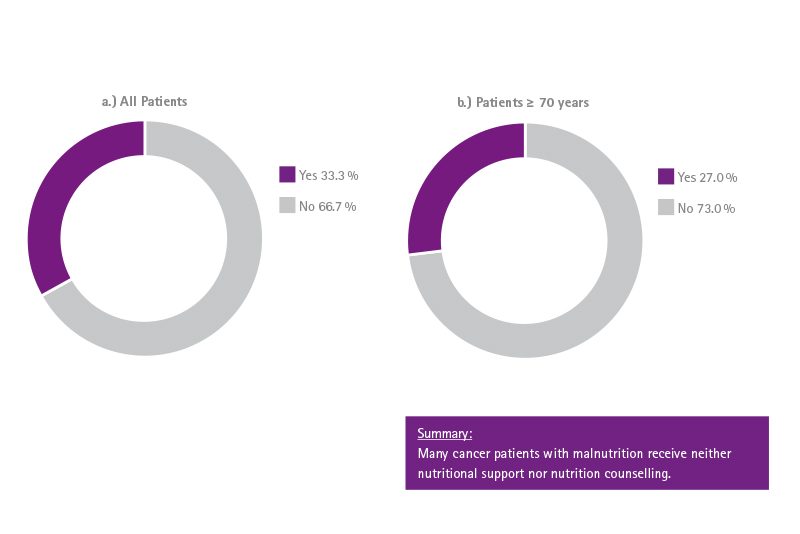
Many cancer patients with malnutrition receive neither nutritional support nor nutrition counseling.5 Nutritional intervention with Oral Nutritional Supplements may improve energy intake and reduce weight loss in cancer patients.1
Why use a patient pathway algorithm for nutrition therapy?
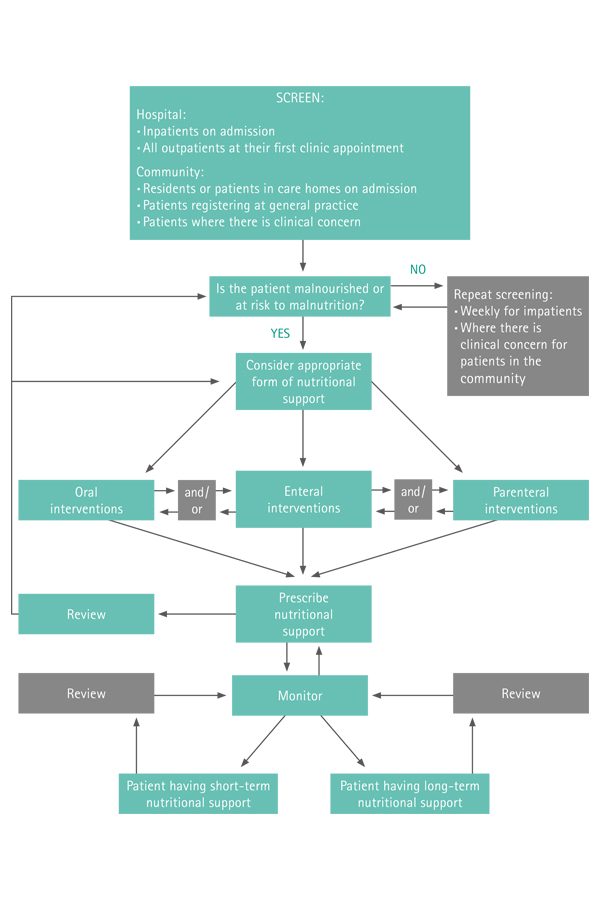
It is essential that healthcare professionals combine their clinical experience and practical common sense with a sound knowledge of the evidence base in the provision of nutritional support.
3 examples:
- A patient with a poor appetite may not be able or willing to consume extra food or may lack the energy or ability to prepare it.
- A patient who has lost the ability to swallow may need tube feeding.
- A patient with intestinal obstruction may need parenteral nutrition.
Patient pathway algorithms are available to assist with decision-making; an example is shown in Fig. 2.9
That means, for a cancer patient, if a decision has been made for nutrition therapy, the first choice should be nutritional counseling by a suitable healthcare professional (e.g., registered dietitians). If oral nutrition remains inadequate despite nutritional interventions (counseling, oral nutritional supplements), enteral nutrition should be chosen. If this is not possible, parenteral nutrition should be considered.1
Outlook: benefits of nutrition therapy in cancer patients
Working with patient pathway algorithms (see graphic 2) showed that nutritional intervention may improve nutritional status and perhaps, therefore, prolong survival.
A retrospective study of women suffering from palliative ovarian cancer showed that improved nutritional status is associated with longer survival. Patients with an improved nutritional status at 3 months had a significantly better survival rate than those with deteriorated nutritional status at 3 months (survival of 18.5 months vs. 3.5 months). That indicates that some patients with malnutrition had the chance with nutritional support to shift to a better nutritional status and might, therefore, have better survival.10
Another study in gastric cancer patients showed similar results. Patients with Nutritional Risk Screening (NRS) > 3 (malnourished) who shifted to a good nutritional status (NRS < 3) after nutritional support lived longer. Young, male and good response to chemotherapy were more likely to have the NRS shift to < 3 after nutritional support. Median survival was 14.3 and 9.6 months for patients with and without NRS shift respectively.11
Nutritional therapy in malnourished or at-risk cancer patients
- may help to improve body weight and energy intake1
- can reduce the incidence of postoperative infectious and non-infectious complications, together with a positive effect on length of hospitalization12
- may improve physical activity and QoL1
- can diminish negative effects of radiotherapy on nutritional status1
- may prolong survival1
- may improve QoL1,13
- may reduce cancer treatment toxicity1,14
Nutritional support plays an important role for malnourished and at-risk cancer patients.
Highlights
References
1 Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36(1):11-48.
2 Arends J, Baracos V, Bertz H, Bozzetti F, Calder PC, Deutz NEP, et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr. 2017;36(5):1187-96.
3 Bozzetti F, Arends J, Lundholm K, Micklewright A, Zurcher G, Muscaritoli M. ESPEN Guidelines on Parenteral Nutrition: non-surgical oncology. Clin Nutr. 2009;28(4):445-54.
4 Hébuterne X, Lemarié E, Michallet M, de Montreuil CB, Schneider SM, Goldwasser F. Prevalence of malnutrition and current use of nutrition support in patients with cancer. JPEN J Parenter Enteral Nutr. 2014;38(2):196-204.
5 Planas M, Alvarez-Hernandez J, Leon-Sanz M, Celaya-Perez S, Araujo K, Garcia de Lorenzo A. Prevalence of hospital malnutrition in cancer patients: a sub-analysis of the PREDyCES(R) study. Support Care Cancer. 2016;24(1):429-35.
6 Pressoir M, Desne S, Berchery D, Rossignol G, Poiree B, Meslier M, et al. Prevalence, risk factors and clinical implications of malnutrition in French Comprehensive Cancer Centres. Br J Cancer. 2010;102(6):966-71.
7 Davidson W, Teleni L, Muller J, Ferguson M, McCarthy AL, Vick J, et al. Malnutrition and chemotherapy-induced nausea and vomiting: implications for practice. Oncology nursing forum. 2012;39(4):E340-5.
8 Gyan E, Raynard B, Durand JP, Lacau Saint Guily J, Gouy S, Movschin ML, et al. Malnutrition in Patients With Cancer: Comparison of Perceptions by Patients, Relatives, and Physicians-Results of the NutriCancer2012 Study. JPEN J Parenter Enteral Nutr. 2018;42(1):255-260.
9 National Collaborating Centre for Acute Care (UK). Nutrition Support for Adults: Oral Nutrition Support, Enteral Tube Feeding and Parenteral Nutrition. London: National Collaborating Centre for Acute Care (UK); February 2006.
10 Gupta D, Lis CG, Vashi PG, Lammersfeld CA. Impact of improved nutritional status on survival in ovarian cancer. Support Care Cancer. 2010;18(3):373-81.
11 Qiu M, Zhou YX, Jin Y, Wang ZX, Wei XL, Han HY, et al. Nutrition support can bring survival benefit to high nutrition risk gastric cancer patients who received chemotherapy. Support Care Cancer. 2015;23(7):1933-9.
12 Yan X, Zhou FX, Lan T, Xu H, Yang XX, Xie CH, et al. Optimal postoperative nutrition support for patients with gastrointestinal malignancy: A systematic review and meta-analysis. Clin Nutr. 2017;36(3):710-21.
13 Borges L, Paiva S, Silveira D, Assuncao M, Gonzalez M. Can nutritional status influence the quality of life of cancer patients?. Revista de Nutricao 2010; 23(5): 745-753.
14 Paccagnella A, Morassutti I, Rosti G. Nutritional intervention for improving treatment tolerance in cancer patients. Curr Opin Oncol. 2011;23(4):322-30.