Blood Exposure
Blood exposure may occur during insertion, handling, and disposal of an IV catheter, where blood may spill onto the bed, floor, shoes, clothing, gloves, or unprotected skin. As a result, clinical activities must be stopped immediately to clean up blood splashes. Bed linens and clothing may need to be changed, skin disinfected, and environment cleaned. In addition to interrupting treatment, the cleaning work requires additional time and is associated with increased costs and annoyance.1
At-risk blood exposures happen when potentially infectious blood comes into contact with mucous membranes or non-intact skin (e.g. skin that is cracked, abraded, or has dermatitis). Since doctors and nursing staff are often unaware of pathogens in the patient's blood, all blood and body fluids should be regarded as potentially infected and disposed of immediately. 2, 3
Did You Know?
According to research, up to 35.9% of all healthcare workers come into involuntary contact with blood or body fluids at least once a year, with 45% of unreported incidents according to a survey of German hospitals.1
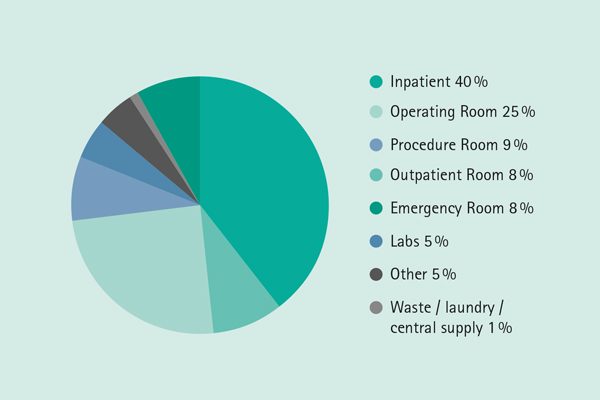
Most exposures to blood and body fluids occur in the patient room (40%), followed by the operating room, treatment room, and emergency room.4
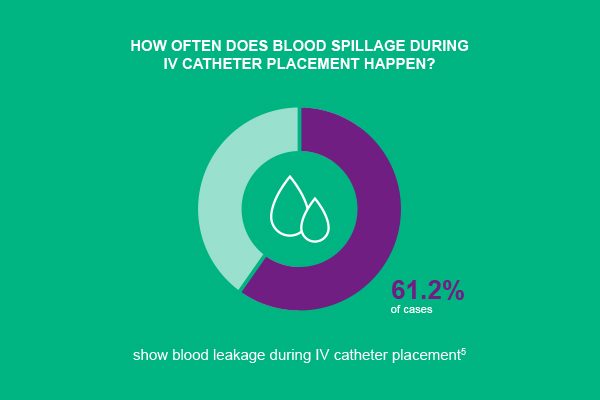
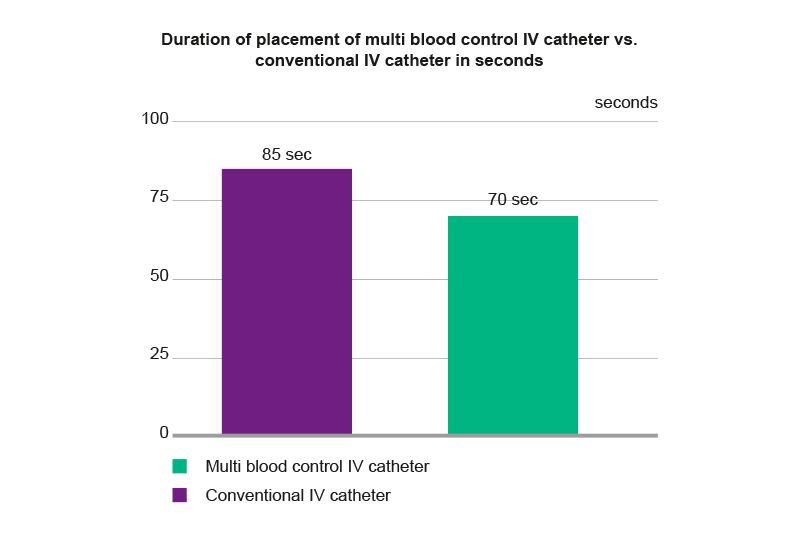
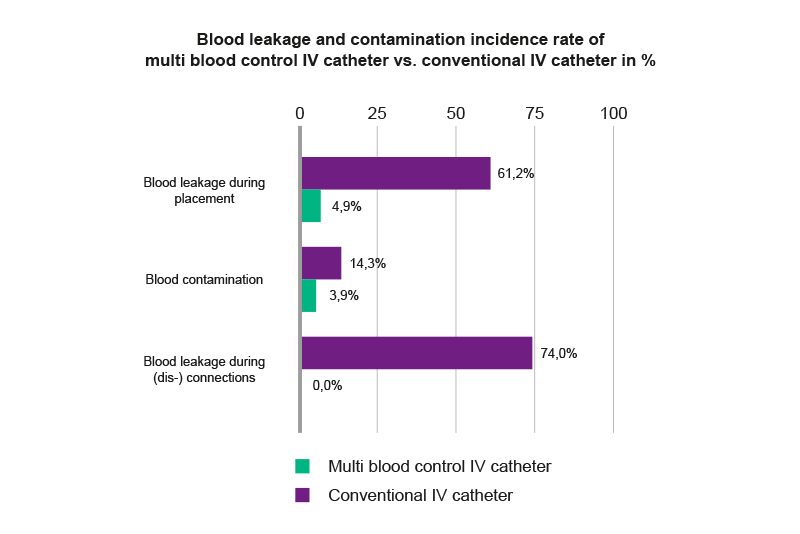
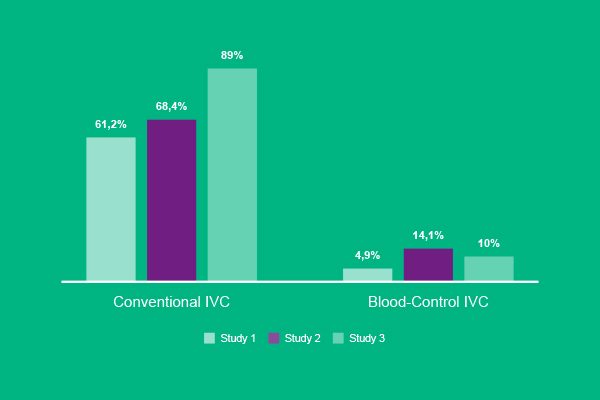
When using conventional catheters, blood leakage can occur in up to 61.2% of cases during insertion and in up to 75% of cases immediately after disconnection. As a result, about one in 7 blood exposures leads to environmental contamination.5
Causes and Challenges
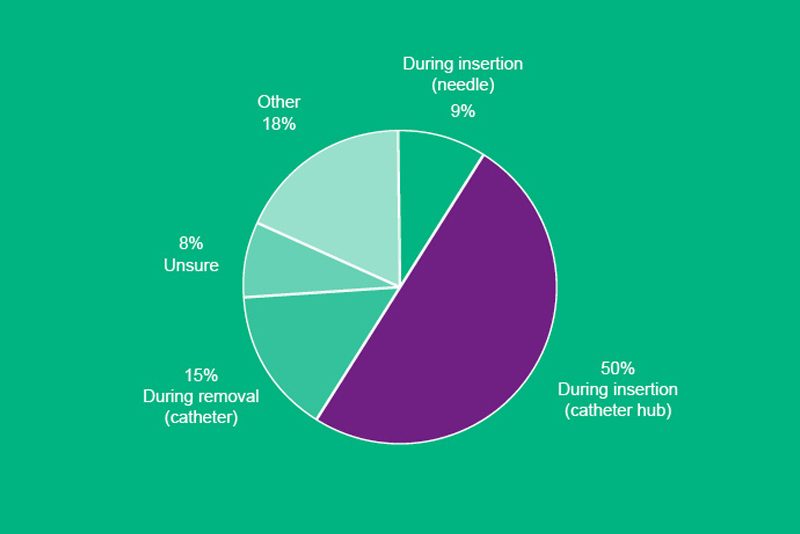
In principle, blood exposure can occur every time a catheter is placed, connected or disconnected to other Luer devices or removed.1
Main causes identified for blood exposure are blood splashes, blood back-flow from catheter hub and insufficient compression of punctured vein during connection and disconnection of Luer devices.1, 5, 6, 7
In addition, the following (environmental) situations may increase the risk of blood exposure:
- High frequency of catheter insertion/removal.
- Hectic work environment, which is especially true in emergency rooms
- Medical staff working under high pressure (stressful situation)
- Low appreciation of the actual work process
The shortage of staff prevailing in hospitals and the resulting time pressure can be observed worldwide. According to a hospital report from Germany, between 1991 and 2010 the number of hospitals and nursing staff was declining, while in parallel the number of patients to be treated was increasing,8 which in turn increases the workload per nurse.
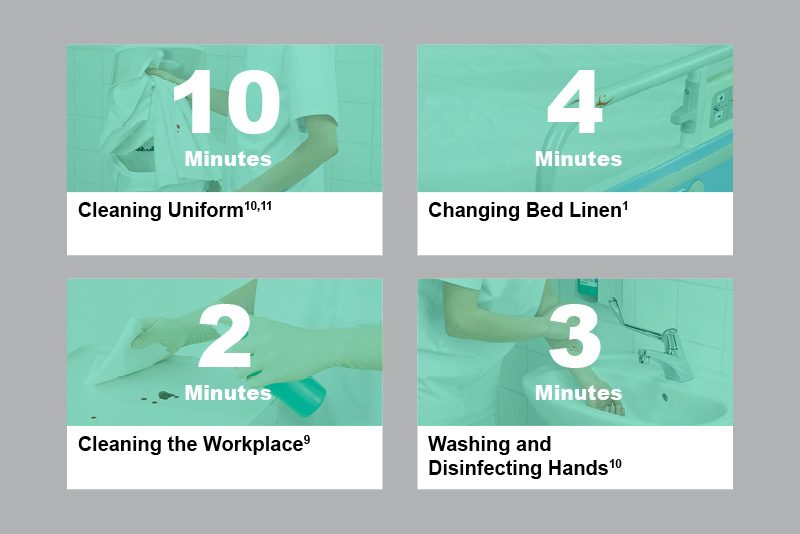
Exposure to blood or spilled blood additionally interrupts the tight workflows of hospital staff and consequently means a not inconsiderable expenditure of time and money for cleaning and disinfection.
When it happens
One study found that blood leaks from the catheter during insertion and removal in about two-thirds of all cases, with catheter placement being by far the most common cause.7
Where it happens
Especially during insertion, handling and disposal of contaminated materials, medical personnel run the risk of unintentional contact with blood.
The risk is further increased when catheter placement is performed on an uncooperative, noncompliant or combative patient.1
Most often, blood spillage can be found on:9
- Armrests
- Baby changing matts/mattresses
- Bed frames and cradles
- Blood pressure equipment
- Examination couches
- Infusion pumps
Consequences
Contact with blood interrupts workflows, involves additional time and is a de facto nuisance - for both medical staff and patients.
In addition to bed linen, clothing might have to be changed, the environment cleaned, and skin disinfected.1 This takes time that is usually not available in the daily hospital routine. The result is a higher stress level and resulting dissatisfaction among staff, but also a lack of understanding among patients, which in turn can affect the hospital's reputation.
The additional tasks resulting from a blood exposure are subsequently lacking in patient care and support.
The financial consequences for this extra effort can be enormous. For example, the average cost of cleaning and disinfection after a blood exposure in a hospital with 4,000 SPIVC per month is $14,000 US per year.1
Preventive Strategies Avoiding Blood Exposure
Preventive measures and protection of clinicians include hand hygiene, wearing personal protective equipment, and using IV catheters with a blood control feature.
Hand hygiene (WHO recommendation)12
- Hand hygiene should be a routine measure
- Hand hygiene should always be performed before and after contact with the patient, and before donning and after removing disposable gloves
- In the event that the nurse’s hands have visibly come into contact with blood or body fluids, hand hygiene should preferably be performed with antiseptic liquid soap and water
Personal protective equipment (PPE)
In addition to wearing personal protective equipment, appropriate cleaning materials should always be within reach1, 7, 13:
- Gloves
- Single-use disposable gown or apron
- Eye protection wear (e. g. goggles, face shield, face mask)
- Material for cleaning and disinfecting (e. g. alcohol wipes, antiseptic wipes, absorbent drapes and sheets, gauze)
Blood Control IV Catheter
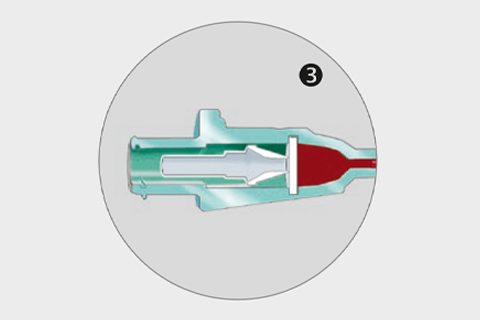
Studies show that blood leakage incidents can be significantly reduced when using IV catheters with a blood control septum.
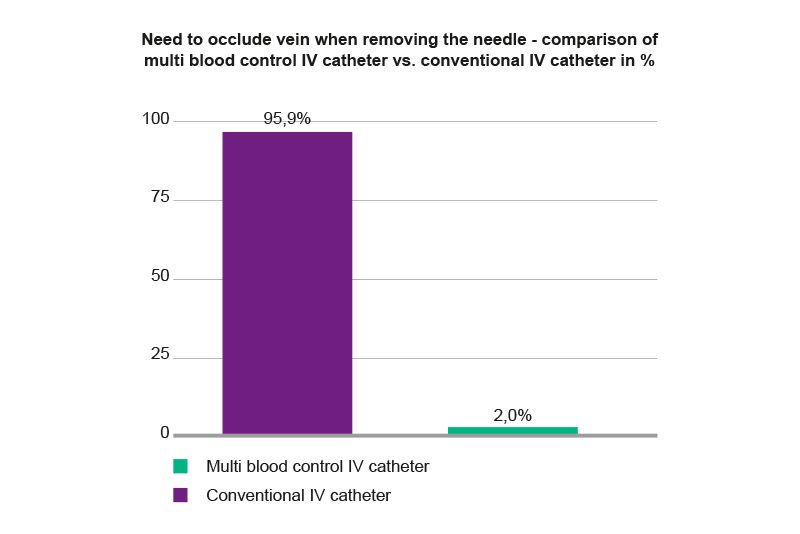
A blood control IV catheter controls the flow of blood coming out of the catheter hub. It reduces both blood exposure during insertion and the need for venous compression, saving cleaning time and materials, while making the whole IV cannulation process easier.
Differences have to be made between one-time (single) and multi-access blood control devices.
One-time (Single) Blood Control versus Multi Blood Control
A one-time blood control septum helps to reduce the occurrence of blood exposure during insertion until first Luer connection is made. Subsequently, vein compression is required for connections and disconnections of Luer devices after initial connection as well as during catheter removal.
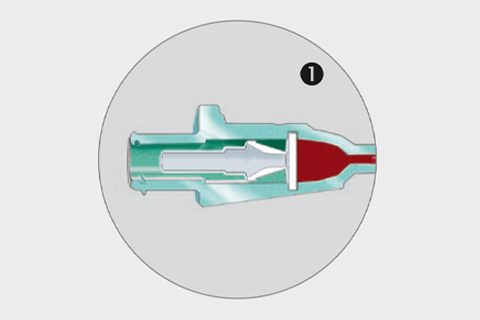
One-time (Single) Blood Control
Septum closed
- Septum is closed when the needle is removed from the catheter hub.
- The septum opener sits behind the septum and blood flow is controlled.
Septum opened
- Septum opens by attaching a Luer device (syringe, IV line, extension line, blood collection device, etc.) to the back of the catheter hub.
- The Luer connection pushes the septum opener; opening the septum completely.
- After initial connection, septum opener remains in septum leaving the catheter open.
The multi blood control septum is designed to control the flow of blood from the catheter hub during needle withdrawal and while exchanging Luer connections, helping to reduce blood exposure occurrence.
A multi blood control septum additionally minimizes blood exposure during disconnecting a device from the catheter hub. This can save approximately 500 minutes per year* in an average size hospital, benefiting patient care.5
* Calculation based on 200,000 catheters placed per year, each saving 15 seconds of time.
Multi Blood Control
Septum closed
- Septum is closed when the needle is removed from the catheter hub.
- The septum opener sits behind the septum and blood flow is controlled.
Septum opened
- Septum opens by attaching a Luer device (syringe, IV line, extension line, blood collection device, etc.) to the back of the catheter hub.
- The Luer connection pushes the septum opener; opening the septum completely.