Difficult Intravenous Access – The daily challenge to hospital staff
Establishing functional peripheral intravenous access is a routine activity in both the emergency department and inpatient setting. While the traditional method of vein palpation for cannulation is successful in the majority of patients, patients with difficult intravenous access (DIVA) present a challenge that hospital staff must address on a daily basis.1
Difficult (peripheral) intravenous access is generally understood as arising when two or more punctures are performed without success, or when puncture support methods are required, or when the impossibility of obtaining peripheral access means that a central venous catheter (CVC) must be inserted.2, 3, 4
They all search for deep veins
Difficult IV access (DIVA) can be expected in the following patients: 2, 3
- Pediatric patients and neonates
- Overweight and obese patients
- Old and chronically ill patients, e. g. those suffering from diabetes
- Emergency and acute care patients who have, for example, skin burns, hematomas, or dehydration
Did You Know?
A difficult IV access is not uncommon. In fact, more than 30% of adults and up to 50% of children requiring a PIVC are found to have a challenging venous access.2
In addition, approximately one-third of critically ill patients are in the group for whom intravenous access can be challenging. These are often patients with generalized edema, obese patients, patients with multiple prior cannulations, or patients who use intravenous drugs. Conventional techniques often fail in these patient groups.5
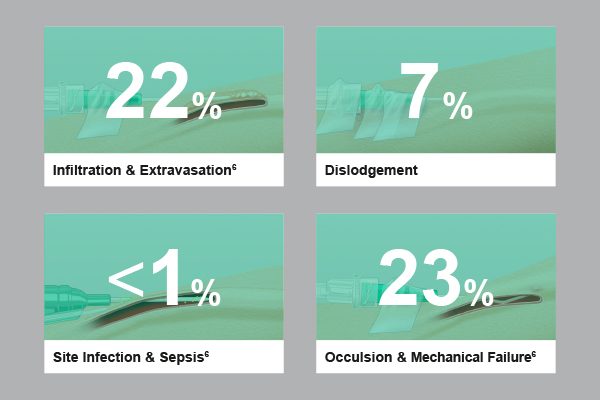
Catheter-related complications further complicate the situation, with an average of 43% of all IV catheters failing.6
In pediatric patients, approximately one-quarter of initially successfully placed IV Catheters had to be removed before the end of therapy due to device failure. This included infiltration at 14.3%, followed by accidental dislodgement (5%) and blockage (2.6%).7
There are a few related characteristics of the cannulated vessel and vascular access device that impact catheter survival: depth of vein, amount of catheter residing in vein, a length of the vascular access.1
Difficult IV accesses take time
The average time required for a peripheral intravenous cannulation is reported to be 2.5 to 13 minutes. Having a difficult IV access it takes up to 30 minutes.3
Causes and Challenges
Overall, the group of patients who are potential candidates for DIVA is large: Neonates and pediatric patients, overweight and obese patients, elderly and chronically ill patients, and acute patients.2, 3
In neonates and pediatric patients, the success rate of correctly placing the catheter on the first puncture is less than 35% due to thicker tissue layers.8 Overall, up to 50% of pediatric patients are considered as DIVA.2
In overweight and obese patients, multiple attempts are usually necessary due to the thicker subcutaneous adipose tissue layer, which in turn is associated with two risks.8, 9 First, the puncture error rate increases, and second, the risk of infiltration is increased. According to the WHO, obesity has nearly tripled worldwide since 1975 and is expected to increase further in Europe.10, 11 Already, 47.6% of European adults are considered overweight and 12.8% are obese.12
Elderly and chronically ill patients, such as those suffering from diabetes, have weaker vascular systems. In the U.S., 14.5% of people are over 65 years old, and 422 million suffer from diabetes.13
Injuries in emergency and acute care patients, such as skin burns, hematomas, or dehydration, result in difficult intravenous access in approximately 11% of all patients.14
„Patients with difficult IV access are frequently subjected to repeated attempts by multiple practitioners. Success rate and time to vascular cannulation are crucial to the optimal resuscitation of a critically ill patient. This can be challenging to even the most experienced emergency nurse.”3
Consequences
Difficult IV access is usually associated with repeated insertion attempts and catheter-related complications. These are not only time-consuming and material-intensive, but also lead to an increased stress level among the nursing staff and the patient, combined with an increased perception of pain.9
Repeated insertion attempts
In the emergency department in particular, the problem of DIVA has been found to negatively impact both patient safety and satisfaction. For example, multiple failed attempts to insert vascular access often result in patients becoming increasingly agitated, exhibiting "needle phobia", and losing trust in healthcare professionals. Patients may develop pain or bruising at the insertion sites, putting them at higher risk for skin injury and infection. Delayed access can further increase the time needed for necessary diagnoses or treatments such as fluid resuscitation and administration of medications or pain medications.2
Complementing this, multiple punctures may be associated with progressive deterioration of the vascular tree, termed "vascular exhaustion", which further complicates vascular access during successive contacts with the patient.15
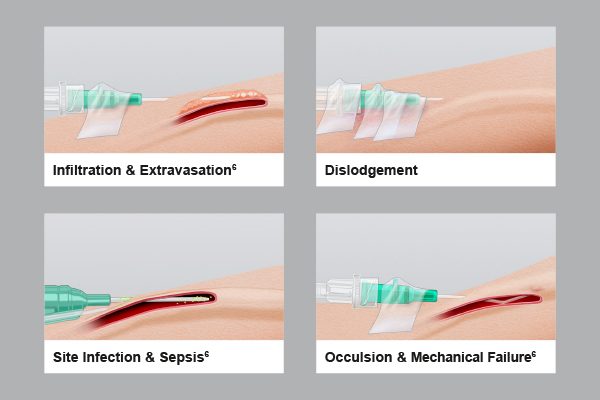
Catheter-related complications
Once cannulated, survival of IV catheters is problematic, with early failure being a common complication.16
Nearly 40% of PIVC are terminated early due to complications such as dislocation and infiltration. Dislocation is when the catheter loses access to the patient's vasculature and causes a forced, premature interruption of infusion therapy. Infiltration, on the other hand, occurs when punctures do not properly target the vascular access and cause the infused solution to flow into the tissue surrounding the vascular access. This complication is particularly relevant when infusing highly irritating (e.g., vesicant) substances.6
In addition to nerves and time, repeated insertion attempts cost material above all. For example, the average cost of replacing PIVCs per sequence of IV treatment is USD 51.92.17
Repeated unsuccessful insertion of a PIVC sometimes leads to switching to more expensive and complex solutions and using central venous catheters (CVC) or peripherally inserted central catheters (PICC). Both alternatives require a longer insertion process and are associated with higher material costs. However, in many cases, CVCs are inserted unnecessarily. Although patients are eligible for a peripheral IV catheter, CVC or PICC are used because of difficult IV access rather than dwell time or infusion solution.18
Preventive Strategies
To treat patients with difficult intravenous access in a time-, nerve-, and material-conserving manner, the use of longer PIVC and ultrasound-assisted catheter insertion is recommended.
Longer length PIVC
A longer part of the capillary tubing stays in the vein and helps to prevent catheter dislodgements and infiltrations.19, 20, 21, 22
It also increases the survival time of the catheter. According to calculations, the optimal length of the catheter in the vein is at least 2.75 cm. Longer length PIVC have a survival time of 129 hours (5.4 days) compared to shorter catheters of 75 hours (3.1 days).16
”A PIVC of appropriate size (gauge and length) should be selected depending on the patient’s veins: the diameter (gauge) is important for patients with very thin veins, while the length is important for obese patients with deep-seated veins.”23
”Longer PIVCs have been observed to have a decreased incidence of infiltration and extravasation, which is especially important when infusing highly irritant (e.g. vesicant) substances.”24
Ultrasound-guided catheter
To identify peripheral vessels and assist in vein cannulation in patients with challenging vein access, ultrasound (US) may be useful.25
“Long catheter US-guided procedure is associated with a lower risk of catheter failure compared with short catheter US-guided procedure.”25
“A longer extended dwell catheter represents a viable and favorable alternative to the standard longer IVs used for US-guided cannulation of veins >1.20 cm in depth. These catheters have significantly improved survival rates with similar insertion success characteristics.”1
Introcan Safety® Deep Access – Handling video of catheter placement – Ultrasound-guided venipuncture.
Highlight Safety Products
Highlight Safety Products
Scientific Evidence