The importance of pressure ulcer prevention
Pressure ulcers are caused if the blood supply to the skin and the underlying tissues is compromised for prolonged periods of time due to mechanical compression of the local vasulature, with ensuing hypoxia and tissue necrosis. Most of the time, pressure ulcers significantly impact the patients’ morbidity, mortality and quality of life.
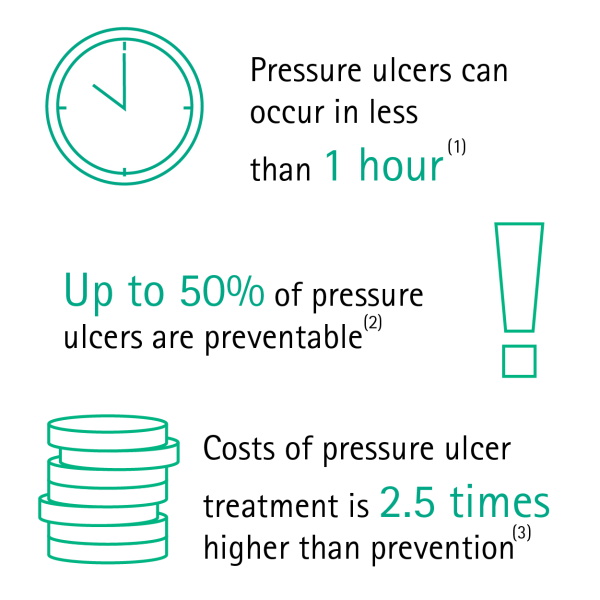
In some cases, these occur quickly - between the first hour and 4 to 6 hours after sustained loading.(1)
Depending on population and ulcer grade, up to 50 percent of pressure injuries can be avoided.(2)
Furthermore, research has proven that the costs of pressure ulcer treatment exceed those of prevention by 2.5 times.(3)
Pressure sore risk areas
Pressure sore risk areas
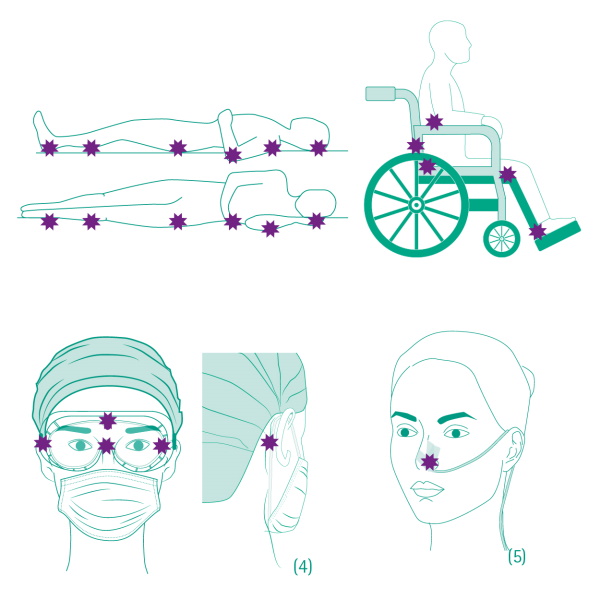
A pressure ulcer is injury to skin or tissue that occurs when blood circulation is decreased because of pressure to a specific area. At first, a slight reddening of the area can be detected. This is referred to as the initial sign of tissue damage.
The sacrum, heels, elbows and shoulder blades are particularly prone to pressure ulcers. In the current medical environment since the outbreak of COVID-19, the face is also extremely at risk of developing pressure ulcers, because health care professionals need to wear personal protective equipment and critical COVID-19 patients are exposed to medical devices related to non-invasive mechanical ventilation.
Preventive measures to adapt
Put a stop to pressure ulcers
Adapt a holistic approach
There are different measures available(6,7) to prevent pressure ulcers. For example, whenever a patient enters a ward, a pressure ulcer risk assessment should be used, followed by a regular skin assessment to check for any signs of sores.
Also, nutrition plays a huge role in the patient’s overall health status influencing the probability of developing pressure injuries. It is important to assess the nutritional needs and adapt the diet accordingly and ensure adequate hydration(7).
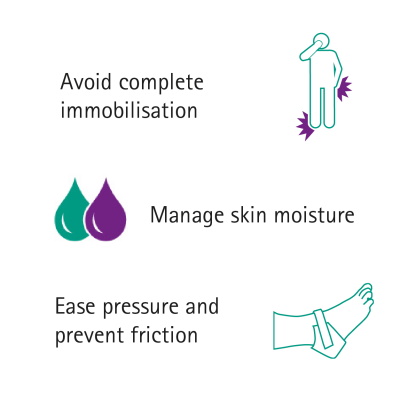
Ease pressure and avoid frictions
But one of the best ways to prevent pressure sores is to change the bed lying position of the patient as much as possible. It is highly recommended to change position and alternate between back and sides at least every two hours. For chairbound patients it is recommended to use a seating surface and to implement weight shifts every 15 minutes.(7)
Specialists(6,7) additionally advise:
- Using prophylactic foam dressings to protect the skin, ease pressure and prevent friction on bony protrusions (e.g. heels, sacrum) or other body parts that are continually exposed to friction and shear.
- Applying skin moisturizer to hydrate dry skin in order to reduce risk of skin breakdown.
- Protecting the skin from excessive moisture exposure with a skin barrier product.
Our solution
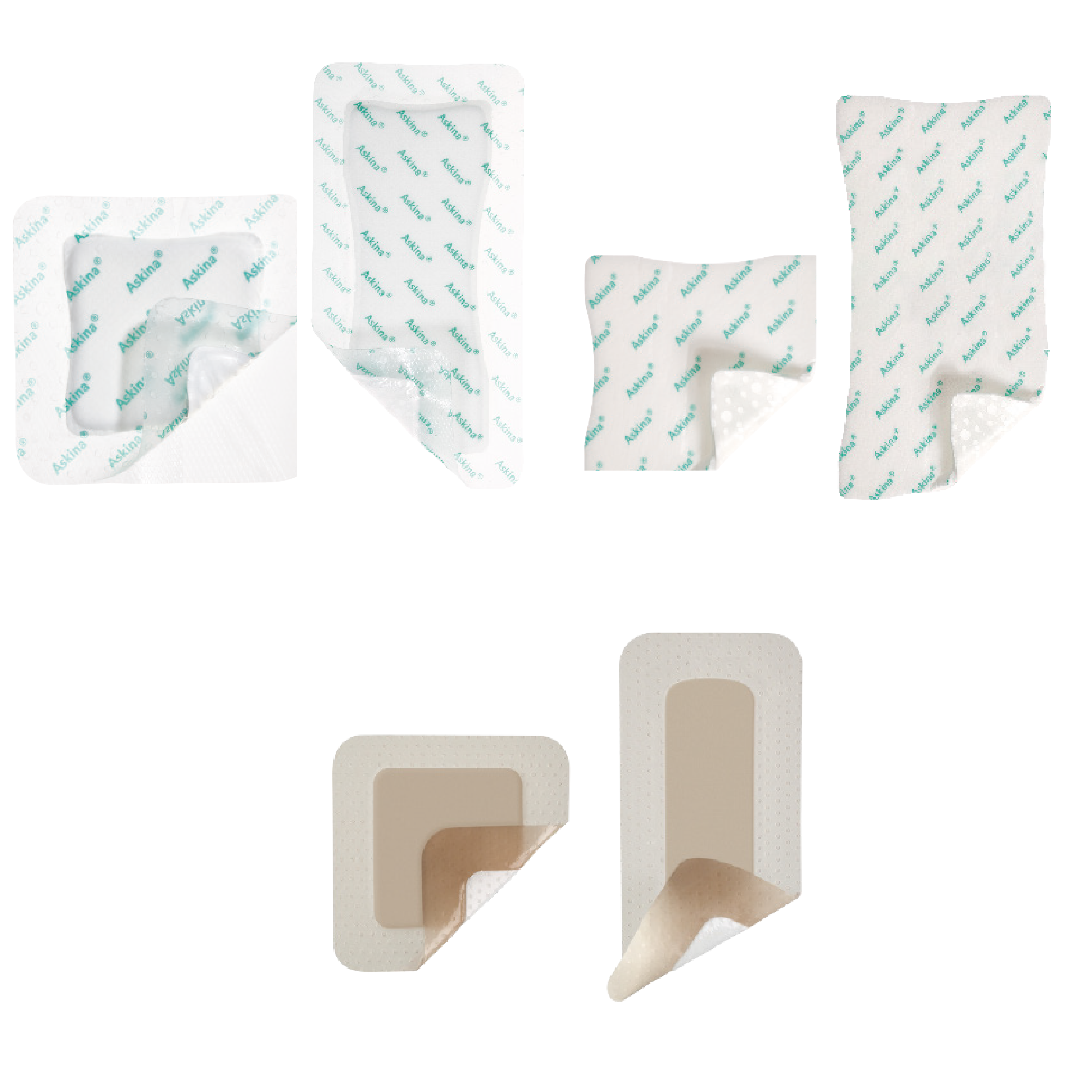
We highly recommend a combination of our soft, cushion-like dressing ranges Askina® DresSil® and Askina® Foam, which relieve pressure and avoid friction, with appropriate local skin moisture management products such as Askina® Barrier and Linovera®.
Less fragile and more resistant - hydrated skin
Linovera® is indicated for prevention and treatment of stage I pressure ulcers. It lubricates the skin, thus reducing shear and friction(7) and maintaining the moisture barrier function of the skin.(8)(9)
The active ingredients of Linovera® are linoleic acid, the most important essential fatty acid for the skin(10), Aloe Vera, which acts as an emollient and a humectant and Centella Asiatica, a soothing skin tonic agent.(11)
Avoid moisture - use a skin barrier product
Skin barrier products are used to manage the level of moisture next to the skin in conjunction with a skin-care routine to keep the skin clean and dry. It is essential to wash the skin using a non-perfumed soap with a natural pH balance.
Askina® Barrier efficiently prevents skin breakdown associated with excessive body fluid exposure. It acts as a lasting protective barrier on patients' skin. When applied, it is quickly absorbed, leaving an invisible breathable water repellent layer, resistant to wash-off. Askina® Barrier is available in three different formats: Askina® Barrier Cream, Askina® Barrier Film Spray or Askina® Barrier Film Swabs. The barrier film may be used on intact or damaged skin particularly at fixation sites for tubes and catheters protecting the periwound areas.
Foam dressings - ease pressure and prevent friction
Areas such as the heels or sacrum are especially exposed non-stop to pressure and friction. Therefore, they need more protection. In addition to applying Askina® Barrier or Linovera® for moisture management anatomically shaped hydrocellular dressings are available to ease pressure.
Askina® Heel, Askina® DresSil® Heel and Askina® DresSil® Sacrum are manufactured to protect the heels, malleoli and the sacrum. Askina® Trachea is a specially designed foam dressing with a circular opening which fits neatly around a tracheostomy tube, stoma or other drain.
Prone to sores – every body part
Bony protrusions are not the only parts of the body which are exposed to pressure and friction. Other parts are affected, too. For example, when a patient is lying in a supine position, which is the preferred position for critical COVID-19 patients.
Askina® DresSil® is a foam with a silicone adhesive which ensures gentle, secure adherence and minimal trauma during dressing changes. It can be cut and shaped for application on smaller areas which need protection.
Askina® DresSil® Border or Askina® DresSil® Border Lite, which are foam dressings with silicone adhesive and an additional adhesive border, are made for difficult-to-dress or moving areas (knees, elbows, skin folds) as they are able to conform to a variety of anatomical contours.
Every foam dressing can be repositioned during application or even lifted up during wear time to check the skin or wound. They can also be applied on wounds as they provide a moist environment promoting natural healing.
Focus on pressure ulcers related to COVID-19 pandemy
COVID-19 patients and the risk of pressure sores
Critical COVID-19 patients with acute respiratory distress syndrome (ARDS) usually require mechanical ventilation performed by endotracheal intubation through the mouth or a tracheostomy. The need to stay still in bed without the opportunity to change position leads to an increased risk of pressure sores.
Health care professionals and the risk of pressure sores
The effectiveness of using personal protective equipment (PPE), such as face masks, goggles and gloves, especially in times of COVID-19 is well known and uncontroversial. But how can you avoid skin lesions, pressure ulcers or friction injuries? We have gathered useful recommendations for you on our dedicated website.
References:
1) Gefen, A. How much time does it take to get a pressure ulcer? Integrated evidence from human, animal, and in vitro studies. HYPERLINK "https://www.ncbi.nlm.nih.gov/pubmed/18927481"Ostomy Wound Manage. 2008 Oct;54(10):26-8, 30-5.
2) Range varies among settings and classification method.
- Bereded DT, Salih MH, Abebe AE. Prevalence and risk factors of pressure ulcer in hospitalized adult patients; a single center study from Ethiopia. BMC Res Notes. 2018;11(1):847. Published 2018 Nov 29. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6267874/
- Vanderwee K, Clark M, Dealey C, Gunningberg L, Defloor T. Pressure ulcer prevalence in Europe: a pilot study. J Eval Clin Pract. 2007;13(2):227-35. (https://www.ncbi.nlm.nih.gov/pubmed/17378869)
- Barrois B, Labalette C, Rousseau P, et al. A national prevalence study of pressure ulcers in French hospital inpatients. J Wound Care. 2008;17(9):373-6, 378-9. (https://www.ncbi.nlm.nih.gov/pubmed/18833894)
- Shahin ES, Dassen T, Halfens RJ. Pressure ulcer prevalence and incidence in intensive care patients: a literature review. Nurs Crit Care. 2008;13(2):71-9 (https://www.ncbi.nlm.nih.gov/pubmed/18289185)
- Vangilder C, Lachenbruch C, Algrim-boyle C, Meyer S. The International Pressure Ulcer Prevalence™ Survey: 2006-2015: A 10-Year Pressure Injury Prevalence and Demographic Trend Analysis by Care Setting. J Wound Ostomy Continence Nurs. 2017;44(1):20-28.(https://www.ncbi.nlm.nih.gov/pubmed/27977509)
3) Chapter 12- Pressure Ulcers: A Patient Safety Issue (2008), Agency for HealthCare Research and Policy (US).
4) Downie, F. & Sandoz, Heidi & Gilroy, P. & Royall, Dawn & Davies, S.. (2013). Are 95% of hospital-acquired pressure ulcers avoidable?. Wounds UK. 9. 16-22.
5) https://www.epuap.org/wp-content/uploads/2016/10/quick-reference-guide-digital-npuap-epuap-pppia-jan2016.pdf
6) Jimenez Torres, J. Acidos Grasos Hiperoxigenados (AGHO) en el tratamiento y prevencion de las ulceras por presion, ulceras vasculares y pie diabetico. Panorama actual del medicamento 2010; 34 (336):695-701
7) Declair V. The usefulness of topical application of essential fatty acids (EFA) to prevent pressure ulcers. Ostomy Wound Manage. 1997;43(5):48-52, 54.
8) Colin D, Chomard D, Bois C, Saumet JL, Desvaux B, Marie M. An evaluation of hyper-oxygenated fatty acid esters in pressure sore management. J Wound Care. 1998;7(2):71-2.